Secrets of Building 7
NIH’s First State-of-the-Art Infectious Disease Laboratory
It was once a proud building filled with innovative scientists who courageously tackled public-health problems. For 60 years, it provided a home for NIH scientists who worked on infectious diseases, identified new viruses, and developed vaccines against hepatitis, rotavirus, and adenoviruses.

OFFICE OF NIH HISTORY
NIH’s Building 7, on the Bethesda campus, boasted a state-of-the-art biosafety system when it opened in 1947: superheated grids sterilized air as it passed through the ventilation system; labs had ultraviolet lights that were turned on each night to sterilize surfaces; access to the laboratories was through decontamination locks; and concrete window canopies instead of fabric shades (that might become contaminated). Above: At night, the building “glows” with ultraviolet light.
Now NIH’s Building 7 on the Bethesda campus awaits demolition, sitting empty and lifeless, a stark contrast for this storied structure that had hosted luminaries in the field of infectious diseases. But oh, what stories the walls could tell.
Infectious-disease research has always been a dangerous proposition. Before the advent of modern biosafety equipment, laboratory-acquired infections were a constant risk for scientists. While not all of these infections were deadly, 10 Public Health Service personnel died as a result of performing or assisting with infectious-disease research between 1928 and 1944. In 1944, two of them died at NIH facilities within six weeks of each other: Richard G. Henderson, in Building 5, of scrub typhus—an acute febrile infectious illness caused by the bacteria Orientia tsutsugamushi; and Rose Parrott, in Baltimore, of tularemia—a rodent-transmitted disease caused by the bacteria Francisella tularensis.
These deaths spurred Congress to appropriate $1.2 million for the construction of a state-of-the-art biosafety facility at NIH to prevent more “martyrs”—scientists who contracted the diseases they were studying and died. Building 7 was originally named “Memorial Laboratory” in honor of Henderson and Parrott. Although the building no longer goes by that name, the road running past it is still called “Memorial Drive.”

Building 7, which has 12-inch steel-reinforced concrete walls, boasted a state-of-the-art biosafety system when it opened in 1947, complete with superheated grids to sterilize air as it passed through the ventilation system and carefully controlled airflow directed from “clean” to “dirty” parts of the building. Ultraviolet lights installed in all labs were turned on each night to help sterilize surfaces.
The only entryways and exits from the laboratories were through decontamination locks, where employees were required to shower and change clothes—coveralls were supplied for wear within the laboratories—before entering the “dirty” labs or the “clean” outside world. The building even had concrete window canopies, obviating the need for internal fabric shades that might become contaminated.

The inhabitants soon realized that there was “one oversight,” recounted the late Robert Chanock in a 2001 oral history interview. He was chief of the Laboratory of Infectious Diseases (LID) in the National Institute of Allergy and Infectious Diseases (NIAID). “They forgot to [seal] the space around the pipes that ran through the building and from one floor to another,” meaning that contaminated air from the infectious-disease laboratories escaped into the rest of the building. The Building 7 researchers were studying Q fever, an infection caused by Coxiella burnetii bacteria that is spread by exposure to infected livestock, and characterized by high fever and pain in the head, neck, chest, and muscles. Most of the researchers, however, had been vaccinated against the disease to avoid becoming accidentally infected.
But only months after the new building opened, there was an outbreak of Q fever that sickened eight unvaccinated victims: five laboratory workers; Joseph Smadel—later the director of Intramural Research at NIH—who only visited the lobby; and the landlords of one of the infected workers—they were exposed to the bacteria when doing their tenant’s laundry. While no fatalities resulted from this outbreak, it was clear that Building 7 was no safer than any other laboratory at the time. In addition, renovations to correct the ventilation defect were impossible without demolishing the building. Despite these defects, it was still the safest possible environment in which to work on infectious diseases in the 1940s.
No further large-scale outbreaks occurred, mostly because the LID ceased research on highly virulent organisms. Individual researchers did, however, acquire nonfatal laboratory-associated infections from time to time. For instance, then–NIAID researcher Richard Wyatt, who worked in the building from 1971 to 1983, was once accidentally infected with norovirus while centrifuging fecal filtrates. Wyatt is currently the deputy director, Office of Intramural Research.
Important research began in Building 7 almost as soon as the first laboratories moved in in 1947. The building’s first inhabitants were LID researchers led by Charles Armstrong, who was already well-known for his work on the prevention of botulism poisoning from improperly canned foods. He also identified the mosquito-borne virus behind the 1933 St. Louis, Missouri, encephalitis outbreak that infected more than 1,000 people within a two-month period.
Another early inhabitant was Robert Huebner—Armstrong’s protegé—who had done extensive fieldwork on Rickettsialpox and Q fever at the behest of the Public Health Service. “Q” stands for “query,” meaning the causative agent was unknown when the disease was discovered in the 1930s; although the pathogen was discovered in 1937, the name stuck. Huebner spent the 1950s in Building 7, analyzing patient samples and isolating 70 new viruses as well as describing the clinical symptoms associated with each.
Alexis Shelokov, another early inhabitant, brought some of the first tissue-culture techniques to NIH, enabling Huebner and others to grow viruses in culture for the first time.
Janet Hartley, later head of the Viral Oncology section of the NIAID’s Laboratory of Viral Diseases, began her scientific career as a bacteriologist in Huebner’s laboratory, where she worked while obtaining her Ph.D. at George Washington University in Washington, D.C.
“In those days in Building 7, all the investigators wore blue jumpsuits. Everybody,” recalled Hartley in a 1995 oral history interview. “I met with Bob Huebner, who was a big man, and his blue jumpsuit was a little too small for him…. But he was so full of enthusiasm for what they were doing—that you know I could think there is no place that I’ve been that I want to work more than this place.”
OFFICE OF NIH HISTORY
Some people concentrate better when they draw—this notebook used by Wallace P. Rowe at a 1960s conference in Europe, seems to attest to that.
The 1950s also brought batches of promising young officers from the Public Health Service to Building 7. Some of them, such as Wallace P. Rowe, who worked with Huebner to help discover adenoviruses and was later chief of the Viral Diseases section, became so enamored of the ongoing research that they spent their careers there.
In 1957, Chanock and Albert Kapikian began their respective laboratories in Building 7; both were personally recruited by Huebner and would continue their work in Building 7 until NIAID built modern biosafe labs in Building 50 many years later. Chanock studied respiratory viruses. In 1962, he identified respiratory syncytial virus (RSV), the most common cause of serious lower respiratory infections in infants. In the 1970s, he developed the first nasal anti-influenza vaccines.

OFFICE OF NIH HISTORY
Albert Kapikian presented important virology research done in his Building 7 laboratory in the 1970s using these lantern slides.
Kapikian studied nonbacterial gastroenteritis and in the early 1970s identified norovirus and rotavirus using the electron microscope in the sub-basement of Building 7. Robert Purcell, who joined LID in 1963, identified the virus that causes hepatitis A in 1973. He eventually developed a vaccine against it that was commercially released in 1995.
“The respiratory viruses were on the third floor, hepatitis was on the second floor, and the diarrhea viruses were on the first floor,” recalled Wyatt, who came to Building 7 as a Public Health Service Fellow in 1971. “So it was almost an anatomical arrangement—from head to lower abdomen.”
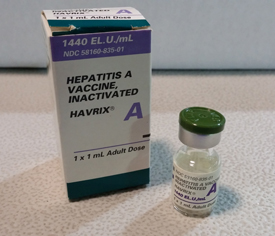
OFFICE OF NIH HISTORY
Robert Purcell, of NIAID’s Laboratory of Infectious Diseases, used an attenuated virus to create the first available Hepatitis A vaccine, HAVRIX, in Building 7.
Permanent staff turnover was low. When Rowe died of colon cancer in 1983 at age 57, the array of laboratory chiefs in Building 7 had remained constant for 15 years. To honor him, a former storage room on the fourth floor was renovated and became the Wallace P. Rowe Conference Room. Even the stairway leading up to the fourth floor was made more attractive: An Art Nouveau–style window depicting a waterfall and matching balusters were installed. Lab meetings were held in the conference room until 2001, when biosafety facilities in Building 50 were completed and NIAID left Building 7. Chanock, Purcell, and Kapikian still led their respective laboratories.
After NIAID left, Building 7 was renovated to provide temporary space for researchers whose own labs were undergoing major renovations. In 2003, the National Eye Institute (NEI) and other laboratories that had been housed in Building 6 moved into Building 7. Although the shower rooms and other remnants of biosafety features were gone, the remaining structural oddities made an impression on the new inhabitants: Closets had doors that led outside; restrooms had unusual proportions because they were once the only entryways to laboratories; the old ventilation system became overloaded when new heating, ventilation, and air conditioning equipment was installed; and the new fans dislodged fine black dust from the vents, which settled over the laboratory benchtops overnight. The conference room fell into disuse—the fire marshals declared it unsafe, citing that the only exit was that single staircase.
As Building 7 was only supposed to be an interim home for the scientists, essential items for daily experiments were constructed on a makeshift basis, such as a darkroom for work on light-sensitive pigments. Due to unforeseen complications, the renovations of Building 6 took twice as long as expected, and NEI labs remained in Building 7 until summer 2009.
In January 2009, a pipe burst in Building 7’s attic, sending sheets of water cascading through the labs on the south side of the building. There was no structural damage to the building, but the water nearly destroyed the expensive equipment sitting on the benchtops and flooded many drawers, ruining what was inside. The toll of age on the pipes was obvious. Because they could not be fixed, plans for other laboratories to move into the building were cancelled. By the end of 2009, NEI and all other occupants were gone…for good.
Building 7 has remained empty ever since. Empty bullet casings, broken glass, and fake blood litter the floors, left over from police use of the vacant building for emergency training drills. The electricity was disconnected five years ago, but a few lights, rigged up by the environmental remediation contractors, shine weakly on the first floor. The carpet in the Wallace P. Rowe conference room on the fourth floor has been partially torn up, and light from the round window highlights the cracked and peeling wallpaper. The only occupants of the building now are the environmental-remediation experts who toil away removing the remains of the old labs. In 2016, the demolition experts are expected to take over (and will demolish nearby Building 9, too) to free up the space for a new research facility.
MORE STORIES ABOUT BUILDING 7
Building 7 Ventilation System
The lack of “airtight” laboratories after Building 7 opened in 1948 was noticed quickly. “The defect was identified by a very simple test that should have been performed at the time the building was accepted from the contractor,” recalled Robert Chanock in a 2001 oral history interview. “The NIH engineers set off a smoke bomb in the sub-basement and 15 seconds later, the smoke was in the attic.”
Investigators also took it upon themselves to test the airflow within the building. “Dr. Armstrong was very skeptical about whether Building 7 was truly germ-proof,” said Edward Beeman (NIAID research fellow from 1948 to 1952) in a 2004 interview. “He did an experiment as follows: He used a bacterium called Serratia marcescens…and put it into one of the exhaust ducts of the building. Theoretically this stuff was supposed to be taken through a series of ducts and out through an incinerator grill that would destroy all the germs. Then Dr. Armstrong left a series of open Petri dishes in the attic of Building 7. Now, this particular organism leaves a distinctly pink colony on a plate in agar, so it was expected to serve as a very efficient marker. After several days, Dr. Armstrong went up to the attic to check his suspicions. I don’t know how many Petri dishes he left, but every single one of them was just loaded with these germs.”
Alligator in the Shower
Long after the showers had outlived their intended purpose, scientists found other ways to use them. Richard Wyatt recalled that alligator blood was required in the Complement Fixation laboratory, so an alligator was kept handy—in one of the showers. Complement fixation is a method used to detect a specific antibody or antigen in a biological sample and requires red blood cells to detect a result. It has largely been replaced by enzyme-linked immunosorbent assay technology.
The Benefit of Crowded Spaces?
As the number of staff working in Building 7 increased throughout the 1970s, the available lab space shrank to a minimum. Even the space around the electron microscope in the sub-basement was at a premium. Richard Wyatt recalled that one day, Dewitt Stetten, the deputy director of intramural research at the time, visited the laboratories. The scientists hoped he would advocate on their behalf for more space. They directed his attention to the cramped conditions and made a point of displaying the crowding around the electron microscope. But Stetten was unimpressed. Upon the conclusion of the visit, he remarked that in his opinion, the best science came out of crowded spaces and left. No more space was allocated to the LID.
Huebner’s Field Work: Rickettsialpox
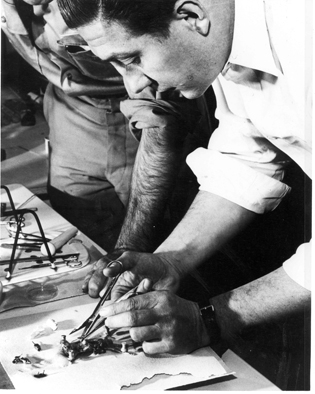
OFFICE OF NIH HISTORY
Robert Huebner at work in the U.S. Public Health Service’s field laboratory in the Kew Gardens apartment complex in New York, 1946. He is using scissors and forceps to dissect a mouse. Of note, protective clothing such as gloves or masks are not in use.
In 1946, the Public Health Service was called upon to investigate an unknown epidemic involving high fevers and rashes in the residents of Kew Gardens, Queens, New York. Because Robert Huebner was the only officer on duty at the time, he was sent to investigate the cause of the epidemic. He traveled to Kew Gardens and took extensive patient samples to bring back to Bethesda, where he successfully isolated an organism called Rickettsia akari, which was similar to other Rickettsia bacteria.
Knowing the causative agent was not enough to stop the epidemic, however. It was also necessary to learn exactly how the disease spread. With the help of an intrepid exterminator named Charles Pomerantz, who observed a massive mite infestation in the buildings where patients lived, Huebner was able to show that the same organism was found in the mites and in human patients and that mite bites could transmit the organism, causing infection. As the mites did not normally have human hosts, Huebner further showed that the mice living in Kew Gardens were a reservoir of the causative organism. This remarkable set of investigations was completed in just under seven months. Extermination of the rodent population and subsequent treatment of patients with antibiotics eliminated Rickettsialpox from the area after several years.
Building 7’s Historical Luminaries
Mentioned in article:
Charles Armstrong (1886–1967): He was the first chief of LID. In addition to his already mentioned work on botulism and St. Louis encephalitis, Armstrong was well known for his work on preventing tetanus infections secondary to smallpox vaccinations and for adapting human poliomyelitis virus to grow in mice and monkeys, facilitating much of the modern research on the disease. He was elected to the National Academy of Sciences in 1944.
Robert Huebner (1914–1998): After investigating epidemics and determining the causative agents, Huebner became interested in the role of viruses in tumor formation. In 1968, he left LID to head the National Cancer Institute’s newly formed Laboratory of Viral Carcinogenesis. He originated the use of the word “oncogene” and provided funding and ideas to leading cancer researchers around the country. He was elected to the National Academy of Sciences in 1960.
Janet Hartley (1930–): Having begun at the NIH in 1953 as a bacteriologist in Robert Huebner’s laboratory while she completed her Ph.D., Hartley became an investigator in her own right, eventually becoming head of the Viral Oncology Section of NIAID’s Laboratory of Viral Diseases in 1983. She retired in 1998 but continued her investigations as emeritus faculty for nearly 10 years.
Alexis Shelokov (1919–): After a colorful childhood in Manchurian Russia, Shelokov emigrated to the United States, where he attended Stanford Medical School in Stanford, California. He brought some of the first tissue-culture techniques to LID, where he worked on poliomyelitis. He introduced the roller-tube technique, which involved growing a monolayer of cells in nutrient media–filled tubes in a rotating drum. He was chief of the Laboratory of Tropical Virology at NIAID in the 1950s and 1960s.
Wallace P. Rowe (1926–1983): He arrived at the NIH as a young Public Health Officer in 1952 and collaborated with Robert Huebner in the discovery of adenoviruses. He later became chief of the Viral Diseases section of NIAID and worked on the role of retroviruses in oncogenesis. He was elected to the National Academy of Sciences in 1975. He died of colon cancer at the age of 57.
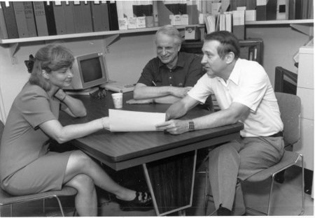
OFFICE OF NIH HISTORY
Vanessa Hirsch, Robert Chanock (center), and Robert Purcell. Hirsch was an investigator for the NIAID’s Laboratory of Infectious Diseases from 1988 to 1996. She subsequently became head of NIAID’s Laboratory of Molecular Microbiology. Chanock was the head of NIAID’s Laboratory of Infectious Diseases while Purcell was the head of NIAID’s Viral Hepatitis Section. (1990s)
Robert Chanock (1924–2010): During his long and illustrious career at NIH, he discovered respiratory syncytial virus, discovered that Mycoplasma pneumoniae caused “walking pneumonia” (which was previously thought to be of viral origin), and developed vaccines against adenovirus infection and the first intranasal influenza vaccine. He became the chief of LID in 1968 and was elected to the National Academy of Sciences in 1973.
Albert Z. Kapikian (1931–2014): Using electron microscopy, he identified the first norovirus, visualized rotavirus, and helped visualize hepatitis A. He also developed the first rotavirus vaccine.
Robert Purcell (1935–): During his 50 years at NIAID, he developed the first animal model for hepatitis B, identified the hepatitis A, D, and E viruses, and worked on the first available vaccine for hepatitis A. He was elected to the National Academy of Sciences in 1988. In addition, he was co-chief of LID with Brian Murphy and retired in 2013.
Richard Wyatt (1942–): As a Public Health Service fellow, he studied gastrointestinal viruses in Building 7 for 12 years before transferring into an administrative role as a special assistant on AIDS-related research. He is currently the deputy director, Office of Intramural Research.
Not mentioned:
Karl Habel (1908–1981): He held several notable positions at NIAID: chief of the Laboratory of Infectious Diseases (1948–1954), chief of the Section on Basic Studies (1954–1959), and chief of the Laboratory of Biological Viruses (1959–1967). He led the poliomyelitis studies that Alexis Shelokov joined when he arrived at NIH. He was elected to the National Academy of Sciences in 1968.
Dorland J. Davis (1911–1990): Director of NIAID from 1964–1975, he worked on a variety of diseases including poliomyelitis and psittacosis. He established nationwide centers for the study of allergic diseases, sexually transmitted diseases, and influenza.
Edward Beeman (1923–2011): He was a Public Health Service fellow in Robert Huebner’s lab from 1948 to 1952, after which he went on to a career in practicing internal medicine. He later authored biographies of Huebner and of Charles Armstrong, and he donated the coveralls seen in this article to the Office of NIH History.
Brian Murphy (1942–): He joined NIH in 1970 and focused his research on developing vaccines for a wide variety of disease-causing viruses: respiratory synctial, parainfluenza, influenza, dengue, and West Nile. He became chief of the respiratory viruses section of LID in 1983, co-chief of LID with Robert Purcell in 2001, and retired in 2010.
Herbert (Sandy) Morse III: He joined the Laboratory of Viral Diseases in 1980 and became chief of LIP in 1985. Worked closely with Janet Hartley in studying the effect of B cells on autoimmunity and neoplastic transformation. In 2011, LIP merged with the Laboratory of Immunogenetics, and he became chief of the Virology and Cellular Immunology Section.
T. Michael Redmond (1957–): He worked in Building 7 from 2003 to 2009 during NEI’s temporary stay there. During that time, his lab studied retinoid metabolism; in particular, their work completed in Building 7 showed that retinal pigment epithelium-specific protein 65kDa (RPE65) is the retinol isomerase enzyme essential for regeneration of visual pigments, and they also determined the biochemical basis of RPE65’s isomerase mechanism, which ended a 20-year controversy in the field. He is the chief of NEI’s Laboratory of Retinal Cell and Molecular Biology.
Patricia Becerra (1953–): She worked in Building 7 from 2003 to 2009 during NEI’s temporary stay there. While in Building 7, she and her lab worked on pigment epithelium-derived factor (PEDF), a protein that acts in neuronal differentiation and survival in the retina and central nervous system. PEDF also has antiangiogenic and antitumorigenic properties. Beccara’s lab found that the retinal pigment epithelium secretes PEDF into the interphotoreceptor matrix, where it acts on photoreceptor cells and maintains its avascularity; and identified a PEDF receptor in the retina. Beccera is the chief of the Section on Protein Structure and Function in NEI’s Laboratory of Retinal Cell and Molecular Biology.
This page was last updated on Tuesday, April 26, 2022
