Subra Suresh: At the Interface of Engineering and Biology
National Science Foundation Director Shares an Engineer’s Perspective on Malaria Research
BY CAROLYN GRAYBEAL, NIAAA
Engineer-scientists have long been intrigued by the physics of large organ systems such as the circulatory system and the skeletal system. But now, they are gaining insights into disease-induced changes in the physical properties of cells and molecules those systems.
National Science Foundation (NSF) director Subra Suresh, an engineer-scientist himself, delivered a special Wednesday Afternoon Lecture on July 25, 2012, that focused on medical advances being made at the intersections of physical sciences, engineering, and biology. Suresh, formerly the dean of the School of Engineering at the Massachusetts Institute of Technology (MIT) in Cambridge, Mass., is particularly interested in malaria.
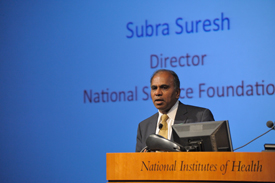
Photo by Branson
Malaria is caused by a small parasite transmitted by the Anopheles mosquito. The parasite enters the bloodstream, infects liver cells, reproduces, and later invades red blood cells (RBCs), causing them to rupture and spew more parasites into the bloodstream. One of malaria’s consequences is blood clots in the brain that occur when the RBCs become so inflexible that they can’t squeeze through the brain’s microvasculature.
Suresh described how he and his colleagues used optical tweezers to measure the RBC’s lost flexibility. First, two reflective beads are adhered to each side of the RBC; a laser is used to trap and pull the beads; and then the force needed to stretch the cell is measured. Scientists had suspected that malaria-infected RBCs lose flexibility and can become three- to four-fold stiffer. Using this engineering technique, however, Suresh showed that the malaria-infected RBCs can become up to 50-fold stiffer.
Suresh showed dramatic video footage of healthy and infected RBCS in action. Healthy, flexible RBCs can change from their natural disk shape into a bullet shape that can shoot across thin capillaries found in the brain. But in the video, two infected, stiff RBGs impeded the flow rate as they sat like boulders, forcing the healthy RBCs to maneuver around them. “Suppose you had [more] of them blocking an entry,” Suresh said. “Would [healthy] blood cells be able to navigate through this [blockage]?”
Suresh is using engineering techniques to make headway in the diagnosis and treatments arenas, too. He and his MIT colleagues harnessed microfluidics technology to design a portable “lab on a chip” that can detect malaria. A drop of blood is placed on the chip; the RBCs flow through an obstacle course of channels of various shapes and sizes. The flow rate provides an indication of the cell’s flexibility, health, and stage of infection.
“I hope I have convinced you [that] there are exciting new possibilities...at the intersections of traditionally disparate fields,” Suresh said in his concluding remarks. “These are interesting approaches [that] can potentially shed significant light [on] the way in which we look at diseases.”
To see the lecture in its entirety, go to https://videocast.nih.gov/ and click on “Past Events.”
This page was last updated on Friday, April 29, 2022
