Research Briefs
Read about Scientific Advances and Discoveries by NIH Intramural Scientists: Quantum computing sifts through genetic haystack; microRNAs play a role in scleroderma; pros and cons of using artificial intelligence to make a diagnosis; using fragmentomics to asses tumor risk; impact of food allergies varies by age; rapid face-detecting circuit discovered; opportunistic infections common in VEXAS syndrome.
NIDDK: NeEDL Finds Links in Genetic Haystack
Many inherited diseases, such as diabetes and Alzheimer’s, may be caused by mutations interacting across multiple genes. With billions of possible mutations that could affect such interactions across the entire genome, however, finding these connections is like searching for the proverbial needle in a haystack. Now, a new tool developed by an international team that includes NIDDK researchers makes the search much easier. Called NeEDL, short for network-based epistasis detection via local search, this tool uses network medicine coupled with quantum computing to identify the most statistically relevant epistatic interactions (EIs) between point mutations called single nucleotide polymorphisms (SNPs).
EIs are a measure of the effect of an interacting group of genetic variations for which the whole effect could be much greater than the sum of its individual parts. Finding the EI between two SNPs is a common lab-based exercise, but finding the EI between five or more SNPs is too computationally daunting, requiring possibly millions of hours to compute on even the fastest supercomputer. To overcome this hurdle, the NeEDL team, led by Markus Hoffmann, a postdoc in the NIDDK lab of Lothar Hennighausen, first turned to a quantum computer at CERN in Switzerland and a support team at the University of Verona in Italy to develop the necessary algorithm upon which NeEDL is based. Quantum computers—rare, expensive to use, and still in the prototype stage—are nevertheless orders of magnitude faster than the fastest supercomputer.
With the algorithms computed, Hoffmann and his team created an EI search engine, of sorts—that is, NeEDL—that researchers can download and use on a fast computer (although, the super-er the better) to find clinically meaningful SNP connections. The free tool can analyze upward of 150,000 SNPs on a supercomputer, such as Biowulf at the NIH. Hoffmann, who created NeEDL as part of his doctoral thesis at the Technical University of Munich (Freising, Germany) and his postdoctoral fellowship at the NIH, said the tool is optimized for quantum computing and would be able to analyze tens of millions of SNPs rather quickly once these next-generation computers are fully developed. For now, NIDDK researchers hope to use the tool to identify possible SNP-based disease connections and then develop the animal models to test the NeEDL output. (NIH authors: M. Hoffmann, S.G. Lee, J. Jankowski, H.K. Lee, and L. Hennighausen, PMID: 39175109)
NIDCR, NHLBI, NCI: DRIVERS AND BIOMARKERS OF SYSTEMIC SCLEROSIS
Systemic sclerosis (SSc), also known as scleroderma, is an autoimmune condition that causes the skin and vital organs such as the lungs to become fibrotic and stiff due to atypical connective tissue growth. A research team led by Wanjun Chen, senior investigator in NIDCR’s Mucosal Immunology Section, discovered a crucial interplay between microRNA-19b (miR-19b) and the cytokine interleukin-9 (IL-9) in the progression of SSc.
MicroRNAs are noncoding RNA molecules that are known to play a role in regulating gene expression in certain tissues and in immune cells. In a series of in vitro experiments, the investigators described a molecular pathway by which miR-19b was upregulated in SSc, driving production of IL-9, a cytokine secreted by helper T cell 9 (Th9) immune cells.
Using a mouse model of SSc, the investigators then showed that inhibiting miR-19b or IL-9 in mice with SSc reduced symptom severity, suggesting that high concentrations of miR-19b boosts the differentiation of Th9 cells, subsequently elevating IL-9 production and contributing to SSc pathogenesis. The scientists found similar mechanisms at play by analyzing gene expression in the cells of patients with SSc.
The findings could offer new therapeutic targets and serve as a biomarker for disease progression, and the authors note that more research is needed to understand the role of Th9-associated pathogenesis in other human diseases. (NIH authors: Y. Lim, S. Park, W. Jin, W.L. Ku, D. Zhang, J. Xu, L.C. Patiño, N. Liu, R. Kazmi, K. Zhao, Y.E. Zhang, and W. Chen, PMID: 39083380)
[BY HÉCTOR CANCEL–ASENCIO, NINDS]
NLM, NEI, CC: STUDY EXPOSES RISKS AND BENEFITS OF INTEGRATING AI INTO CLINICAL SETTINGS

CREDIT: NLM
GPT-4V, an AI model, often made mistakes when describing the medical image and explaining its reasoning behind the diagnosis, even in cases where it made the correct final choice.
A multimodal artificial intelligence (AI) model known as Generative Pre-trained Transformer 4 with Vision (GPT-4V) can analyze both text and visual inputs. NIH researchers and their extramural colleagues found that this model can perform comparatively to human physicians in making a diagnosis based on medical images and associated clinical notes, but it exhibited flaws in its performance. According to the authors, the study builds on prior research that found that GPT-4V can accurately answer multiple-choice questions but did not thoroughly assess whether the model was using the correct underlying rationale.
The researchers tasked GPT-4V and physicians with answering 207 multiple-choice questions from the New England Journal of Medicine Image Challenge, an online quiz that presents medical images alongside a short description describing a patient’s symptoms and then asks users to select the correct diagnosis. Investigators analyzed the model’s proficiency in answering questions and its rationale within the three categories of image comprehension, medical knowledge recall, and step-by-step reasoning.
GPT-4V had a slightly higher overall accuracy in choosing the correct diagnosis (81.6%) compared to physicians (77.8%); however, the model had flawed rationale in 35.5% of the cases in which it nevertheless made the correct choice. Errors in the image comprehension category were particularly prominent. “Understanding the risks and limitations of this technology is essential to harnessing its potential in medicine,” said Zhiyong Lu, senior investigator and corresponding author of the study, in a press release. (NIH authors: Q. Jin, R. Summers, M. Chiang, and Z. Lu, PMID: 39043988)
[BY MELANIE BARKSDALE, NIAID]
NCI: DNA FRAGMENTOMICS IDENTIFIES RISK OF PERIPHERAL NERVE SHEATH TUMORS
A team of pediatric oncology researchers from NCI and their university and hospital collaborators developed a noninvasive method for assessing tumor risk in patients with neurofibromatosis type 1 (NF1).
NF1 is a genetic disorder caused by mutations in the gene for neurofibromin 1, which is essential for normal cell function. In the absence of this protein, peripheral nerve sheath tumors (PNSTs) can grow along nerves. These tumors can be malignant, classifying NF1 as a cancer predisposition syndrome.
The NCI-led team found that DNA fragmentomics—a novel technique for extracting biomarker information from blood-derived DNA fragments—is effective for early detection and risk assessment of PNSTs. The investigators extracted and sequenced cell-free DNA from blood samples of 101 patients with NF1 and 21 healthy control subjects. The resulting DNA fragments were then analyzed and used to successfully classify the tumors as benign, premalignant, or malignant.
The authors note that the findings could enhance early cancer detection and intervention, leading to better outcomes for individuals with NF1 at risk of developing malignant tumors. (NIH authors: R.T. Sundby, A. Pan, S.Z. Mahmood, O.H. Reid, B. Murray, S. Patel, A.N. Lucas, M. Fagan, A. Dufek, E. Dombi, A.M. Gross, B.C. Widemann, and J.F. Shern, PMID: 39093127)
[BY MEAGAN MARKS, NIAAA]
NIAID: FACTORS INFLUENCING QUALITY OF LIFE IN PATIENTS WITH FOOD ALLERGY VARY BY AGE
CREDIT: NIAID
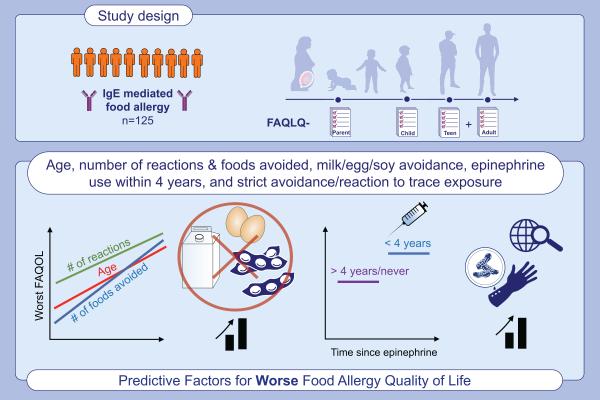
Researchers identified multiple factors that influence quality of life in people with food allergy, and they found the relative impact of those variables varied according to age.
NIAID investigators have conducted a comprehensive study reviewing validated age-specific questionnaires to identify key predictors of quality of life of people with food allergies.
Because food allergies, broadly speaking, has no cure, effective individualized treatments can only be developed and implemented if factors having the greatest influence on psychosocial wellbeing at different ages are well understood, according to Pamela Frischmeyer-Guerrerio, chief of NIAID’s Laboratory of Allergic Diseases and senior author on the study, published in the journal Allergy.
Frischmeyer-Guerrerio's team analyzed questionnaire responses from 125 participants between the ages of 2 and 28 years with physician-diagnosed immunoglobulin E-mediated food allergies. Poor quality of life was associated with increasing age, stricter avoidance practices, and more severe reactions. Other predictors of quality of life included the timing and number of reactions and type and number of foods avoided, with allergies to milk, egg, soy, sesame, or wheat having a particularly negative impact on quality of life. Moreover, the relative impact of those factors varied according to age.
Upcoming work will examine parents’ distress regarding their child’s food allergies. “A better understanding of the factors affecting the parental burden of having a child with food allergy, and how these factors relate to those [variables] affecting the quality of life of the child, will be essential for clinicians to optimally support families with food allergy,” Frischmeyer-Guerrerio told the Catalyst. (NIH authors: S.A. Kubala [now Children's Hospital of Philadelphia], F.D. Young, V. Callier, M.M. Rasooly [now University of Maryland Medical System], C. Dempsey, E. Brittain, and P.A. Frischmeyer-Guerrerio, PMID: 39096008)
[BY SEPPIDEH SAMI, CC]
NEI: NEW FACE-DETECTING NEURONS IDENTIFIED
The brain’s ability to selectively recognize faces out of a field of visual information is thought to be processed within specialized populations of neurons known as “face patch” regions in the visual cortex. Deepening our understanding of this facial processing, researchers at NEI have identified a new, fast-acting face-detecting population of brain neurons. This newly identified circuit, located in the midbrain superior colliculus (SC), responds rapidly to faces and can detect faces in the periphery.
The research team recorded neuronal activity in rhesus macaques (Macaca mulatta) when images of face and non-face objects were shown in the monkey’s peripheral visual field. They observed face-related responses in the SC that followed the presentation of visual cues by 40 milliseconds, significantly faster than face patch regions, and distinguished facial stimuli from other objects with nearly 80% accuracy. Further analysis revealed that SC neurons may receive their inputs from early visual processing regions in the cortex.
According to the authors, the findings suggest that neurons in the SC may serve as an early facial detection mechanism that steers visual focus to facial stimuli, in contrast to other face-selective regions that may serve to process facial information with greater detail. (NIH authors: G. Yu, L.N. Katz, C. Quaia, A. Messinger, and R.J. Krauzlis, PMID: 38959893)
[BY ASHLEY PRATT, NICHD]
NIAMS, NHLBI, NIAID, NHGRI, NCI, CC: OPPORTUNISTIC INFECTIONS ASSOCIATED WITH VEXAS SYNDROME RAISE MORTALITY RISK, PRESENT PREVENTION STRATEGIES
CREDIT: NIAMS
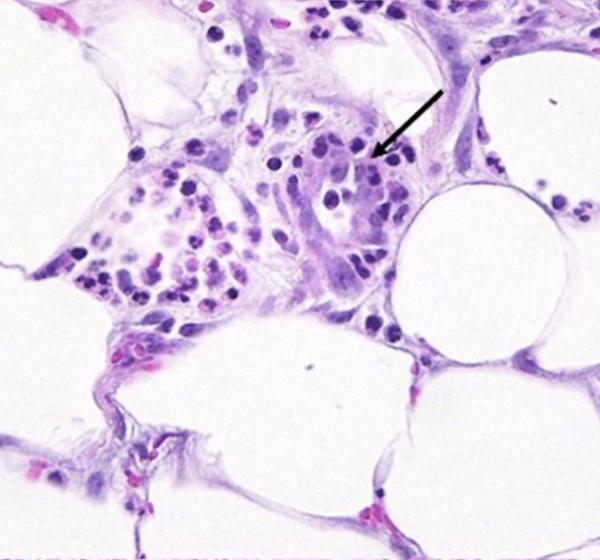
Patients with VEXAS syndrome are at risk for opportunistic infections and can develop inflammation that affects multiple organs. Shown is neutrophilic infiltration in a blood vessel wall (arrow) in the subcutaneous skin adjacent to an area of dense acute inflammation in a person with VEXAS syndrome.
Researchers continue to understand and develop treatments for VEXAS syndrome, a genetic disorder first described by NIH scientists in 2020 (PMID: 33108101). VEXAS is caused by mutations in the UBA1 gene that can lead to bone marrow dysfunction and inflammatory symptoms affecting multiple organs. A multi-IC study led by NIAMS identified opportunistic infections associated with increased mortality that are common among patients with VEXAS but for which prophylactic treatment for some of those infections is markedly effective.
Of 94 patients with VEXAS in this study, 26 developed infections including nontuberculous mycobacteria (NTM), reactivation of varicella zoster virus (VZV) or herpes simplex virus (HSV), and Pneumocystis jirovecii pneumonia (PJP). Increased mortality rates occurred in individuals who developed NTM, HSV, or PJP, but not those who had VZV. Furthermore, prophylactic treatments for PJP and VZV were found to be highly effective in preventing infection.
According to the authors, the findings suggest that management of some patients with VEXAS should include early involvement of infectious-disease specialists. (NIH authors: M. Czech, J. Cuellar-Rodriguez, B.A. Patel, E.M. Groarke, E.W. Cowen, B. Turturice, D.B. Beck, L. Wilson, W. Goodspeed, I. Darden, N.S. Young, D. Hickstein, A. Ombrello, P. Hoffman, E.A. Arikan, N. Sinaii, L. Hathaway, L. Castelo-Soccio, A. Fike, D.B. Kastner, P.C. Grayson, and M.A. Ferrada [now University of Maryland School of Medicine], PMID: 39077052)
This page was last updated on Thursday, December 5, 2024
