Mariana J. Kaplan, M.D.
NIH Distinguished Investigator
Systemic Autoimmunity Branch
NIAMS
Research Topics
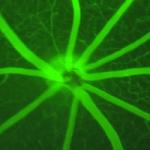
Dr. Kaplan's research has focused on identifying mechanisms of immune dysregulation, organ damage, and premature vascular disease in systemic autoimmunity. Specifically, she investigates how innate immunity (in particular, type I interferons and myeloid cells) promotes autoimmune responses and end-organ damage in systemic lupus erythematosus, rheumatoid arthritis, and other systemic autoimmune diseases. Recently, her research has focused on identifying abnormalities of neutrophil subsets and the role of neutrophil extracellular traps (NETs) in systemic autoimmune disorders, both of which may contribute to the development of autoimmune responses and end-organ damage. Dr. Kaplan is also interested in identifying novel therapeutic targets that may prevent premature vascular damage in systemic autoimmunity and the role of environmental triggers in the induction of autoimmunity. Moreover, she has led clinical trials to identify mechanisms that reduce blood vessel dysfunction and mitigate organ damage in autoimmune and chronic inflammatory disorders.
Biography
Mariana Kaplan, M.D., joined the NIAMS as Chief of the Systemic Autoimmunity Branch in 2013. She is also a Deputy Scientific Director. Before her appointment, she was a Professor of Medicine in the Division of Rheumatology at the University of Michigan. Dr. Kaplan obtained her medical degree at the National Autonomous University of Mexico and did her Internal Medicine Residency at the National Institute of Medical Sciences and Nutrition in Mexico City. She then completed her Rheumatology Fellowship and postdoctoral training at the University of Michigan, where she was a faculty member for 15 years and an active member of their Multidisciplinary Lupus Clinic.
In addition to her research activities, Dr. Kaplan is an active clinician and teacher. She sees lupus patients at the NIH Clinical Research Center and is involved in developing various clinical trials for patients with autoimmune diseases at the NIH. She has served in numerous roles at the American College of Rheumatology/Rheumatology Research Foundation, the American Association of Immunologists, and the Lupus Foundation of America. Dr. Kaplan was inducted into the American Society for Clinical Investigation (ASCI) and the Association of American Physicians (AAP) in addition to receiving the Henry Kunkel Young Investigator Award, the Edmund L. Dubois Memorial Lectureship, and the 2021 Distinguished Basic/Translational Investigator Award, all from the American College of Rheumatology. She received the 2015 Evelyn V. Hess Award from the Lupus Foundation of America in recognition of her significant contributions to lupus research, diagnosis, and treatment. In 2016, she received the Charles L. Christian Award for significant impact on the understanding of lupus. Dr. Kaplan served on the editorial board of the Journal of Immunology and Journal of Clinical Investigation and is deputy editor of Arthritis & Rheumatology. She is currently a Council member at the AAP.
In 2021, she was elected to the National Academy of Medicine for seminal contributions that have significantly advanced the understanding of the pathogenic role of the innate immune system in systemic autoimmune diseases, atherosclerosis, and immune-mediated vasculopathies.
In 2023, Dr. Kaplan was designated NIH Distinguished Investigator. NIH Distinguished Investigators have established a record of career-high achievements and are considered NIH’s most preeminent Senior Investigators (top 2-3%). Entrance requires a special peer review and approval by the NIH director.
Selected Publications
- Carmona-Rivera C, Zhang Y, Dobbs K, Markowitz TE, Dalgard CL, Oler AJ, Claybaugh DR, Draper D, Truong M, Delmonte OM, Licciardi F, Ramenghi U, Crescenzio N, Imberti L, Sottini A, Quaresima V, Fiorini C, Discepolo V, Lo Vecchio A, Guarino A, Pierri L, Catzola A, Biondi A, Bonfanti P, Poli Harlowe MC, Espinosa Y, Astudillo C, Rey-Jurado E, Vial C, de la Cruz J, Gonzalez R, Pinera C, Mays JW, Ng A, Platt A, NIH COVID Autopsy Consortium, COVID STORM Clinicians, Drolet B, Moon J, Cowen EW, Kenney H, Weber SE, Castagnoli R, Magliocco M, Stack MA, Montealegre G, Barron K, Fink DL, Kuhns DB, Hewitt SM, Arkin LM, Chertow DS, Su HC, Notarangelo LD, Kaplan MJ. Multicenter analysis of neutrophil extracellular trap dysregulation in adult and pediatric COVID-19. JCI Insight. 2022;7(16).
- Gupta S, Nakabo S, Blanco LP, O'Neil LJ, Wigerblad G, Goel RR, Mistry P, Jiang K, Carmona-Rivera C, Chan DW, Wang X, Pedersen HL, Gadkari M, Howe KN, Naz F, Dell'Orso S, Hasni SA, Dempsey C, Buscetta A, Frischmeyer-Guerrerio PA, Kruszka P, Muenke M, Franco LM, Sun HW, Kaplan MJ. Sex differences in neutrophil biology modulate response to type I interferons and immunometabolism. Proc Natl Acad Sci U S A. 2020;117(28):16481-16491.
- Kim J, Gupta R, Blanco LP, Yang S, Shteinfer-Kuzmine A, Wang K, Zhu J, Yoon HE, Wang X, Kerkhofs M, Kang H, Brown AL, Park SJ, Xu X, Zandee van Rilland E, Kim MK, Cohen JI, Kaplan MJ, Shoshan-Barmatz V, Chung JH. VDAC oligomers form mitochondrial pores to release mtDNA fragments and promote lupus-like disease. Science. 2019;366(6472):1531-1536.
- Carmona-Rivera C, Carlucci PM, Moore E, Lingampalli N, Uchtenhagen H, James E, Liu Y, Bicker KL, Wahamaa H, Hoffmann V, Catrina AI, Thompson P, Buckner JH, Robinson WH, Fox DA, Kaplan MJ. Synovial fibroblast-neutrophil interactions promote pathogenic adaptive immunity in rheumatoid arthritis. Sci Immunol. 2017;2(10).
- Lood C, Blanco LP, Purmalek MM, Carmona-Rivera C, De Ravin SS, Smith CK, Malech HL, Ledbetter JA, Elkon KB, Kaplan MJ. Neutrophil extracellular traps enriched in oxidized mitochondrial DNA are interferogenic and contribute to lupus-like disease. Nat Med. 2016;22(2):146-53.
Related Scientific Focus Areas



Molecular Biology and Biochemistry
View additional Principal Investigators in Molecular Biology and Biochemistry

This page was last updated on Thursday, August 29, 2024