
Brian P. Brooks, M.D., Ph.D.
Senior Investigator
Pediatric, Developmental & Genetic Ophthalmology Section
NEI
Research Topics
The goal of Dr. Brooks' research is to understand the causes and mechanisms of inherited eye diseases especially those that affect children--and to use that knowledge to develop prevention strategies and treatments. Currently, his lab is focused on two diseases: 1) uveal coloboma and 2) albinism. Uveal coloboma is a potentially-blinding congenital eye malformation. Sometimes uveal coloboma occurs in isolation; sometimes, it is associated with other systemic findings (syndromic coloboma.) Most often, coloboma presents sporadically in families, but there are also cases where coloboma can be directly inherited through a parent. Although we have understood the process in eye embryology that leads to coloboma (optic fissure closure), the precise mechanisms by which this process occurs are still largely unknown. Moreover, although mutations in multiple genes have been associated with coloboma, most cases are genetically unexplained. These observations make genetic counseling and molecular diagnosis difficult in a clinical setting. The goal of this research is to better understand the genetic causes of coloboma and to apply this knowledge in a clinical setting to patients and their families. Albinism is an inherited disorder associated with reduced melanin pigment in the hair, skin and/or eyes. Children with albinism usually have reduced visual acuity and nystagmus (an involuntary rhythmic shaking of the eyes). Although children with albinism frequently require glasses, spectacles or contact lenses usually cannot fully correct their vision because the area of the retina that gives people their best visual acuity, the fovea, does not develop normally. The goal of our research is to better understand how a defect in melanin pigment formation leads to fovea formation and to find treatments that might improve pigmentation (and thereby possibly improve vision) in patients with albinism.
Biography
Dr. Brooks graduated summa cum laude, with general honors and honors in zoology, from the University of Maryland. He was supported during his training in the MD, PhD. program at the University of Pennsylvania by the Medical Scientist Training Program. Residency training in ophthalmology and a fellowship in pediatric ophthalmology were completed at the University of Michigan. Dr. Brooks completed a fellowship in medical genetics at the National Human Genome Research Institute and is board-certified by the American College of Medical Genetics and the American Board of Ophthalmology. He has published numerous articles and book chapters on the genetics of eye disease and has received numerous awards, including the Presidential Early Career Award for Science and Engineering (PECASE), the nation's highest honor for young investigators.
Selected Publications
- Lahrouchi N, George A, Ratbi I, Schneider R, Elalaoui SC, Moosa S, Bharti S, Sharma R, Abu-Asab M, Onojafe F, Adadi N, Lodder EM, Laarabi FZ, Lamsyah Y, Elorch H, Chebbar I, Postma AV, Lougaris V, Plebani A, Altmueller J, Kyrieleis H, Meiner V, McNeill H, Bharti K, Lyonnet S, Wollnik B, Henrion-Caude A, Berraho A, Hildebrandt F, Bezzina CR, Brooks BP, Sefiani A. Homozygous frameshift mutations in FAT1 cause a syndrome characterized by colobomatous-microphthalmia, ptosis, nephropathy and syndactyly. Nat Commun. 2019;10(1):1180.
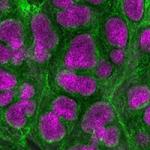
- George A, Sharma R, Pfister T, Abu-Asab M, Hotaling N, Bose D, DeYoung C, Chang J, Adams DR, Cogliati T, Bharti K, Brooks BP. In vitro disease modeling of oculocutaneous albinism type 1 and 2 using human induced pluripotent stem cell-derived retinal pigment epithelium. Stem Cell Reports. 2022;17(1):173-186.
- George A, Zand DJ, Hufnagel RB, Sharma R, Sergeev YV, Legare JM, Rice GM, Scott Schwoerer JA, Rius M, Tetri L, Gamm DM, Bharti K, Brooks BP. Biallelic Mutations in MITF Cause Coloboma, Osteopetrosis, Microphthalmia, Macrocephaly, Albinism, and Deafness. Am J Hum Genet. 2016;99(6):1388-1394.
- Onojafe IF, Adams DR, Simeonov DR, Zhang J, Chan CC, Bernardini IM, Sergeev YV, Dolinska MB, Alur RP, Brilliant MH, Gahl WA, Brooks BP. Nitisinone improves eye and skin pigmentation defects in a mouse model of oculocutaneous albinism. J Clin Invest. 2011;121(10):3914-23.
- Brown JD, Dutta S, Bharti K, Bonner RF, Munson PJ, Dawid IB, Akhtar AL, Onojafe IF, Alur RP, Gross JM, Hejtmancik JF, Jiao X, Chan WY, Brooks BP. Expression profiling during ocular development identifies 2 Nlz genes with a critical role in optic fissure closure. Proc Natl Acad Sci U S A. 2009;106(5):1462-7.
Related Scientific Focus Areas




Molecular Biology and Biochemistry
View additional Principal Investigators in Molecular Biology and Biochemistry
This page was last updated on Friday, August 1, 2025