Reprogramming Cancer
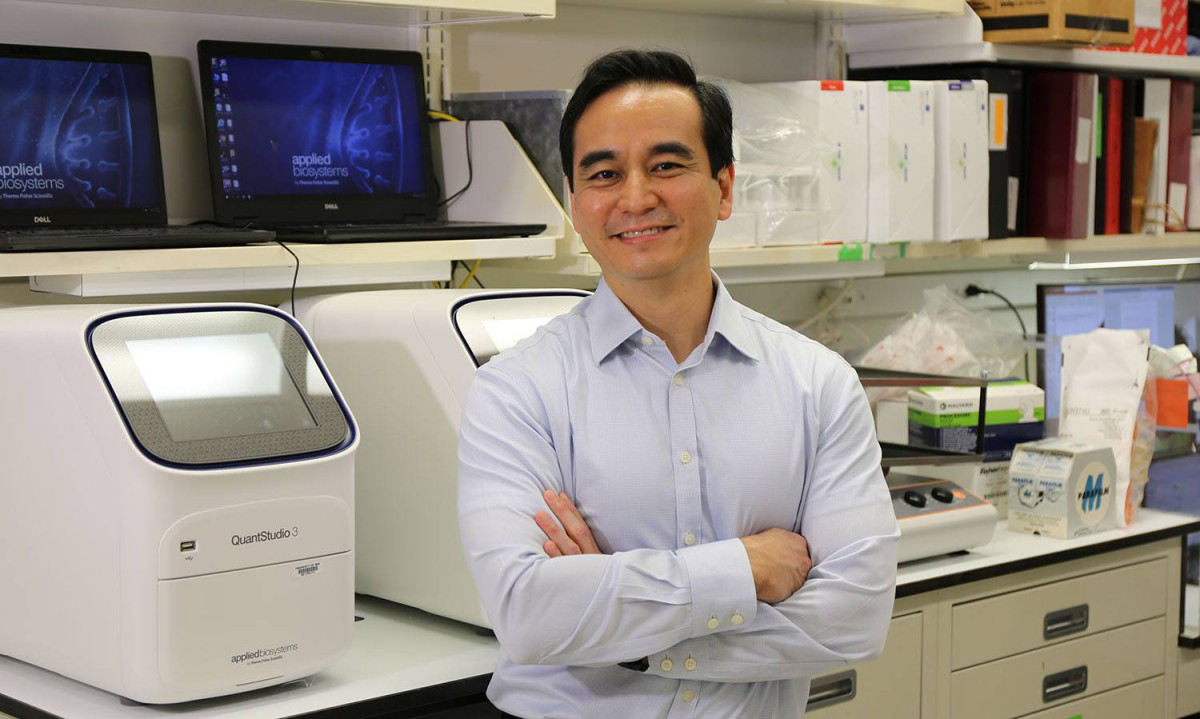
David Takeda is laying the groundwork for a bold new approach to cancer therapy.
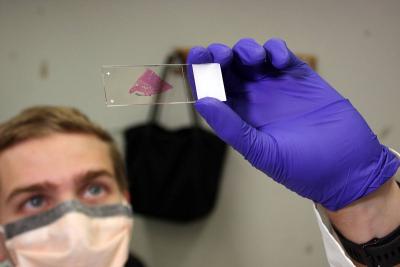
Postbaccalaureate fellow Ben Hauk examines a stained slice of a patient’s tumor.
The human body contains many types of cells that carry out a wide array of tasks: heart cells that beat, neurons that fire off electrical signals, liver cells that filter toxins from the blood. These functional differences result not from differences in the cells’ DNA but rather from ‘epigenetic’ variations, reversible modifications to DNA that do not change its sequence. Epigenetic changes influence gene expression, the process that transforms DNA’s genetic instructions into the proteins cells use to carry out their functions. Just like turning up or down, or even muting, the volume on your television doesn’t change the characters’ dialogue, epigenetic changes can alter how much protein a gene produces without changing the genetic instructions themselves.
Unlike healthy cells, cancer cells have undergone mutations that alter the sequence of their DNA and cause them to grow out of control. What’s more, they can leverage the sorts of epigenetic modifications that affect their healthy brethren in order to thwart treatment. However, IRP investigator David Takeda, M.D., Ph.D., believes that manipulating epigenetics could also provide a powerful new pathway for combatting the disease.

Clinical research fellow Andre Kydd prepares a chunk of a patient’s tumor for epigenetic sequencing by first dipping it in liquid nitrogen to deep-freeze it.
“Instead of thinking about cancer in terms of the mutated genes that drive their abnormal growth and division, perhaps we can reprogram the cell’s state,” he explains. “A cancer cell is a cell that is no longer, say, a skin cell. It’s now a new type of cell that can grow unrestricted. Maybe we can epigenetically reprogram the cell and give it a set of instructions so that it turns into something else — something that you can treat.”
After being selected as a 2019 NIH Lasker Clinical Research Scholar, Dr. Takeda departed the Dana-Farber Cancer Institute in Boston, Massachusetts, to set up the Functional Genomics Section in the Laboratory of Genitourinary Pathogenesis at the National Cancer Institute (NCI). His NIH lab focuses on prostate cancer, and not just because of his prior experience with that cancer at Dana Farber.
Compared to other forms of cancer, prostate cancer’s engine of growth is fairly straightforward. Prostate cancer cells are highly dependent on the androgen receptor, the cellular protein that testosterone must bind to in order to exert its effects. Without testosterone, prostate tumors shrink, which is why prostate cancer that has spread throughout the body is typically treated with androgen deprivation therapy, which cuts off the cancer’s supply of testosterone. This relative simplicity makes prostate cancer a good place to start when exploring the still largely theoretical possibility of combating cancer by manipulating epigenetics.
Still, prostate cancer has been difficult to cure because it frequently becomes resistant to androgen deprivation therapy. The treatment may initially shrink patient’s tumors, but eventually they come roaring back, at which point little can be done.

Postdoctoral fellow Sasha Adamovich prepares prostate cancer cells for an experiment.
“Prostate cancer is not like other cancers where we don’t know what the main driver is,” Dr. Takeda says. “In prostate cancer, we know the androgen receptor is the main driver, but even though we know that, we still can’t cure it.”
Prostate cancer relies on two strategies to overcome a scarcity of testosterone. Scientists have known for some time that treatment-resistant prostate cancer cells have more copies of the androgen receptor gene than treatment-sensitive cells. However, while working at Dana Farber, Dr. Takeda led a study showing that prostate cancer cells can also turn on a regulatory region in their DNA, called an enhancer, that revs up production of the androgen receptor. This adaptation, which is epigenetic because the DNA sequence remains unchanged, allows prostate cancer to thrive even when there is very little testosterone around. The study also demonstrated that shutting down the enhancer slowed down the cancer’s growth.
Dr. Takeda is now following up on this discovery in his lab at NIH. If he can figure out how prostate cancers switch this enhancer on, he theorizes, perhaps he could make treatment-resistant prostate cancer responsive to androgen deprivation therapy once again by turning the enhancer off. At this point, though, that’s just a theory; the cancer may just adopt another strategy to thwart treatment.

Dr. Takeda with members of his lab. From left: Dr. Takeda, Andre Kydd, Shin-Ai Lee, Clara Seo, Ben Hauk, and Sasha Adamovich.
“The question is whether there’s an infinite amount of escape routes, and if you keep blocking these paths, the tumor will just find another one,” Dr. Takeda explains. “But maybe not — maybe there’s only so many routes a tumor can take.”
His efforts to answer that question are only just beginning, as safety restrictions and supply chain bottlenecks related to the COVID-19 pandemic hampered the process of getting his new lab at NIH up and running. Having now overcome those hurdles, his IRP team is poised to make discoveries over the next few years that could spark a brand-new field of epigenetic therapy for cancer.
“Can you tell a cancer cell what to do?” wonders Dr. Takeda. “It would be really cool if you could program a cancer cell to do something. You could dictate its identity epigenetically, and maybe you could change it to a state that’s amenable to treatment or a state where it doesn’t grow, but we don’t yet know if that’s possible.”
“That’s kind of what NIH is for: to try out these big ideas to see if they could possibly work,” he continues. “If it turns out to not work, at least we thought big.”
David Takeda, M.D., Ph.D., is a Lasker Clinical Research Scholar and the head of the Functional Genomics Section in the Laboratory of Genitourinary Pathogenesis at the National Cancer Institute (NCI).
This page was last updated on Wednesday, May 24, 2023