Chronic Plus Binge: A Better Model of Alcohol Abuse
Bin Gao probes the immune system to prevent and treat advanced liver disease.
Dr. Bin Gao (right) and visiting fellow Adeline Bertola, Ph.D. (center), discuss microscope slides containing samples of liver tissues.
While many people may enjoy an occasional alcoholic beverage, excessive alcohol consumption causes adverse effects on the body and mind, including changes in mood and behavior, as well as damage to the liver, heart, and pancreas. Not all chronic alcohol users go on to develop advanced liver disease (ALD), but for the 30-40 percent of heavy drinkers who develop severe liver damage—such as alcoholic hepatitis, cirrhosis, and hepatocellular carcinoma (the most common type of liver cancer)—the current lack of effective treatment strategies is sobering.
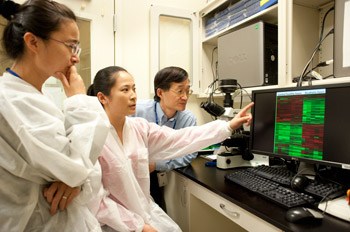
Visiting fellows Man Li, MD., Ph.D. (left), Yan Cai, M.D., Ph.D. (center), and Dr. Gao examine results of microarray analysis of gene expression from alcoholic livers.
“While there are effective drugs for other types of liver disease, such as viral hepatitis, the pathogenesis for alcoholic liver damage is still not clear, and there are no approved therapies for ALD,” explains Bin Gao, M.D., Ph.D., Chief of the NIH’s Laboratory of Liver Diseases. “We’re working on multiple research projects at the cellular and molecular level to give us the foundational knowledge to change that.”
Gao’s research centers around the immune system, the body’s central mechanism in regulating tissue response to the kind of damage that alcohol induces. One cell type of particular interest to Gao is the natural killer (NK) cell, which, as the name implies, is an immune cell that can destroy virus-infected cells and tumor cells without activation by accessory immune cells or antibodies. Gao and his team discovered that NK cells play a critical role in controlling the liver response to damage by killing the activated hepatic stellate cells responsible for liver fibrosis, an intermediate stage in the progression of liver disease to cirrhosis and liver cancer. Chronic consumption of alcohol inhibits NK cells, thereby accelerating liver disease progression.

Prior to examination, mouse liver samples must be encased in wax and then sliced and fixed to a glass slide for viewing.
Shifting focus from immune cells to immune system signaling molecules known as cytokines, Gao’s team searches for cytokines that could have therapeutic potential in ALD by protecting against liver damage and promoting liver cell proliferation. Cytokines are notoriously difficult to regulate from a therapeutic perspective due to their ubiquitous nature in the body, so when Gao and his colleagues demonstrated that the cytokine interleukin 6 (IL-6) plays a critical role in both liver cell protection and proliferation, they knew it would not be a viable therapeutic target for treating ALD, because treatment with this cytokine would have many side effects by targeting all types of cells in the body.

Dr. Bertola (left) and postdoctoral fellow Teresa Ramirez, Ph.D., prepare experiments together at the bench.
Unperturbed, Gao continued to search for a cytokine that could be a viable target, and subsequently discovered that another hepatoprotective cytokine, interleukin-22 (IL-22), helps prevent hepatocyte damage and promotes regeneration by specifically targeting hepatocytes without affecting immune cells. This molecule has now shown promise in Phase I clinical trials as a potential treatment for acute liver failure such as in alcoholic hepatitis.
Most recently, Gao’s group developed an improved animal model of ALD that is fast replacing the standard ‘chronic alcoholic liver injury model’ in use for the past 40 years. While widely used, the old model, in which mice were given an alcohol-based diet for four to six weeks, did not correlate well to the alcoholic liver damage observed in humans.
Dr. Gao and research fellow Dechun Feng, Ph.D., monitor flow cytometry measurement of various types of immune cells in alcoholic livers.
Gao’s new approach, termed the ‘chronic plus binge model,’ uses an alcohol diet for 10 days followed by a single high dose of alcohol that replicates a drinking binge. This pattern is very similar to that seen in many patients with alcoholic hepatitis. The ‘Gao Model’ has already had a profound influence on the ways scientists study alcoholic liver damage, but its impact extends far beyond ALD. Other researchers are now adopting it to study alcohol-induced damage in other organs, such as the pancreas, heart, and kidneys.
The team, happy in the lab
Gao credits some of his team’s success to the freedom inherent to working within the NIH IRP, where they can quickly change course based on new information.
“Simply put, this multidirectional approach to our research probably wouldn’t have been possible anywhere else,” he says. “Here, we have the flexibility to explore multiple lines of research in a more organic way.”
Bin Gao, M.D., Ph.D., is a Senior Investigator and Chief of the Laboratory of Liver Diseases at the National Institute on Alcohol Abuse and Alcoholism (NIAAA).
This page was last updated on Wednesday, May 24, 2023