Probiotic markedly reduces S. aureus colonization in Phase 2 trial
NIH study provides new insights on role of gut in staph colonization
A promising approach to control Staphylococcus aureus bacterial colonization in people — using a probiotic instead of antibiotics — was safe and highly effective in a Phase 2 clinical trial. The new study, reported in The Lancet Microbe, found that the probiotic Bacillus subtilis markedly reduced S. aureus colonization in trial participants without harming the gut microbiota, which includes bacteria that can benefit people. The research was conducted by researchers at the National Institutes of Health led by Michael Otto, Ph.D., an NIH senior investigator at the National Institute of Allergy and Infectious Diseases (NIAID).
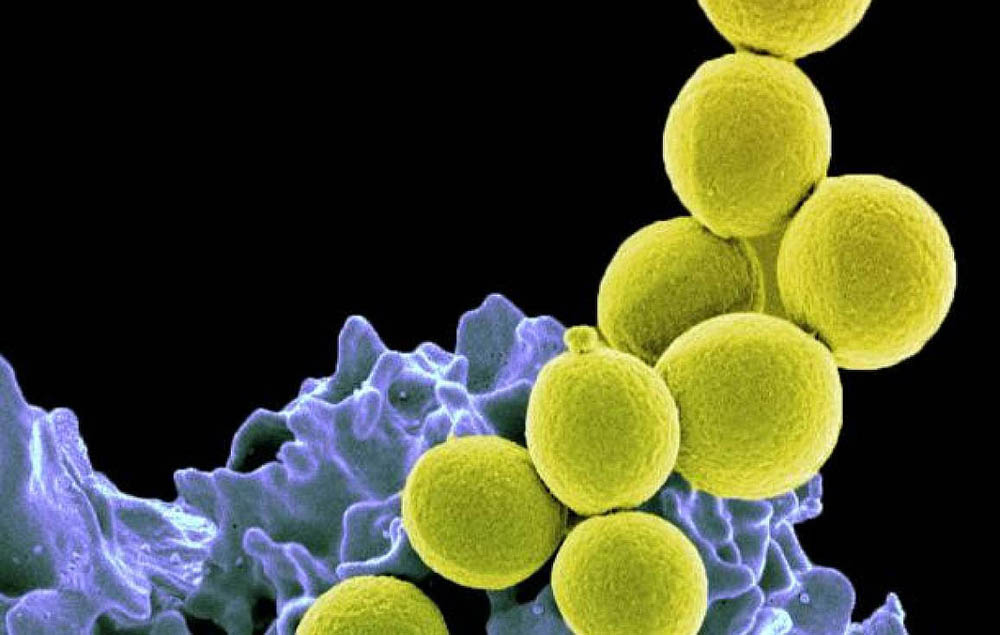
Methicillin-resistant S. aureus, or MRSA, is familiar to many people as a cause of serious disease. Less well known is that S. aureus often lives in the nose, on the body and in the gut without causing any harm. However, if the skin barrier is broken, or the immune system compromised, these colonizing bacteria can cause serious skin, bone, lung, and blood infections.
The prevention of S. aureus infections using approaches to 'decolonize' the body has gained increased attention as the spread of antibiotic resistance limits treatment options. Some decolonization strategies are controversial because they also require large amounts of antibiotics, raising concerns about damage to the microbiota and the development of antibiotic resistance. So far, it appears that only nasal S. aureus colonization can be targeted with topical antibiotics without doing too much harm, but bacteria quickly can recolonize in the nose from the gut.
This page was last updated on Wednesday, January 18, 2023