Research Topics
HIV-1 Replication, Host Restriction Factors, Antiviral Drug Resistance, and Development of Novel Therapeutics
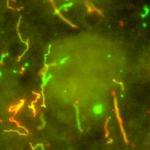
Project 1. Elucidate HIV-1 replication in infected cells by high-resolution live-cell microscopy. Many aspects of HIV-1 replication in infected cells, including nuclear import and capsid dissembly, which are essential for HIV-1 replication, remain poorly understood. To gain insights into these essential steps during HIV-1 replication in infected cells, we developed a new method to label viral complexes by fluorescently tagging APOBEC3F, which is incorporated into virions. Using this method, we showed that reverse transcription is not required for nuclear import of viral complexes, and that HIV-1 capsid interactions with host proteins are essential for nuclear import of HIV-1 capsids (Burdick et al., PNAS 2013). The dynamics and regulation of HIV-1 nuclear import and its intranuclear movements after import had not been previously studied. We carried out high-resolution live-cell microscopy studies of APOBEC3F-labeled viral complexes to determine the dynamics of HIV-1 nuclear envelope docking, nuclear import, and intranuclear movements by live-cell microscopy (Burdick et al., PLoS Pathog. 2017). For several decades, retroviral core uncoating has been thought to occur in the cytoplasm in coordination with reverse transcription or at the nuclear envelope during nuclear import, but no studies have concluded that uncoating occurs in the nucleus. We developed methods to study HIV-1 uncoating by direct labeling and quantification of viral capsid protein associated with infectious capsids. Our results show that intact (or nearly intact) viral cores enter the nucleus through a mechanism involving interactions with host protein cleavage and polyadenylation specificity factor 6 (CPSF6), complete reverse transcription in the nucleus before uncoating, and uncoat less than 1.5 hours before integration near their genomic integration sites. These results fundamentally change our current understanding of HIV-1 post-entry replication events including mechanisms of nuclear import, uncoating, reverse transcription, integration, and evasion of innate immunity (Burdick et al., PNAS 2020).
Project 2. Elucidate the structure and function of APOBEC3 proteins and develop new strategies to treat and functionally cure HIV-1 infection. Our goal is to understand the structure and function of human restriction factor APOBEC3 proteins, which are an important innate immune defense mechanism that protects against invading pathogens. APOBEC3 proteins potently inhibit HIV-1 replication in the absence of the virally encoded Vif protein by incorporating into virions in the virus producing cells and inducing lethal G-to-A hypermutation of the viral DNA in infected target cells. Vif overcomes these host defenses by targeting the APOBEC3 proteins for proteasomal degradation. We have significantly contributed to elucidating the APOBEC3 and Vif determinants that interact with each other (Xu et al., PNAS 2004; Russell & Pathak, J. Virol. 2007; Smith & Pathak, J. Virol. 2010). We have shown that A3G and A3F both inhibit viral DNA integration, but through distinctly different mechanisms (Mbisa et al., J. Virol. 2007; Mbisa et al., J. Virol. 2010). We also developed a bimolecular fluorescence complementation assay to visualize A3G and A3F molecular interactions in living cells and observed that A3G and A3F multimerization, A3G-Gag interactions, and A3G virion incorporation require RNA binding (Friew et al., Retrovirology 2009). We compared the antiviral activity of A3G and A3F in primary CD4+ T cells and macrophages, the natural target cells of infection, and found that while both can inhibit HIV-1 replication A3G is a more potent inhibitor of HIV-1 than A3F (Chaipan et al., J. Virol. 2013).
Recently, in collaboration with Dr. Yong Xiong (Yale University), we determined the structure of a Vif-APOBEC3F-CTD-CBFb complex (Hu et al., Nat. Struct. Mol. Biol. 2020). We demonstrated that APOBEC3 proteins potently induce lethal hypermutation and contribute minimally to viral genetic variation (Delviks-Frankenberry et al., PLoS Pathog 2016). We are developing lentiviral vectors that can efficiently deliver the Vif1-resistant APOBEC3G to hematopoietic stem cells, with the goal of providing a proof of concept that delivering Vif-resistant APOBEC3G to infected patients can provide an approach for a functional cure for HIV-1 infection (Delviks-Frankenberry et al., Mol. Ther. Nucleic Acids 2019).
Project 3. Define mechanisms that confer resistance to nucleoside and nonnucleoside reverse transcriptase (RT) inhibitors. Based on our previous observations on RT template switching and recombination, we proposed that the relative polymerase and RNase H activities of RT can affect the balance between RNA degradation and nucleotide excision, and that mutations that reduce RNase H activities can enhance resistance to nucleoside as well as nonnucleoside RT inhibitors. We observed that several mutations that reduce RNase H activity affect the balance between RNA degradation and nucleotide excision and enhance nucleoside RT inhibitor resistance (Nikolenko et al., PNAS 2005; Nikolenko et al., PNAS 2007; Delviks-Frankenberry et al., PNAS 2008). Our studies have demonstrated that mutations in the connection and RNase H domains also increase resistance to nonnucleoside RT inhibitors, and suggest a parallel mechanism by which resistance to both classes of RT inhibitors can be increased (Nikolenko et al., J. Virol. 2010). These hypotheses were validated by characterization of RT mutations observed in patients and subsequently confirmed by other labs.
Project 4. Demonstrate that xenotropic murine leukemia virus-related virus (XMRV) is a laboratory recombinant and not a human pathogen. XMRV, a gammaretrovirus, was reportedly found in prostate cancer and chronic fatigue syndrome (CFS) patients at high frequencies and thought to be a human pathogen. However, we found that XMRV replication is severely restricted by human APOBEC3 proteins (Paprotka et al., J. Virol. 2010), and its replication is severely restricted in human peripheral blood mononuclear cells, raising doubts about its pathogenicity in humans (Chaipan et al., J. Virol. 2011). To gain insights into the origin of XMRV, we analyzed prostate cancer xenografts that were passaged in nude mice and used to develop a XMRV-positive human cancer cell line. The results showed that XMRV is most likely a recombinant between two murine endogenous proviruses that we named PreXMRV-1 and PreXMRV-2 (Paprotka et al., Science 2011). We concluded that the association between XMRV and human disease is due to contamination of human samples with a laboratory recombinant virus.
Pathak Lab, March 2022
Biography
Dr. Vinay K. Pathak received his B.A. in Biology from the University of California, Los Angeles, in 1979. He obtained his M.S. in Comparative Pathology in 1983 from the University of California, Davis, for characterization of mouse mammary tumor virus proviral integration sites near the int1 and int2 loci in mammary tumors and hyperplastic tissues in Dr. Robert Cardiff's laboratory. He received his Ph.D. for work on characterization of the eukaryotic protein synthesis initiation factors eIF-2α and eIF-2β in Dr. John W.B. Hershey's laboratory at the University of California, Davis, in 1988. He was a postdoctoral fellow under the guidance of Dr. Howard Temin from 1988 to 1991, where he determined the in vivo forward mutation rate of spleen necrosis virus and characterized the nature of mutations that arise during retroviral replication. These studies were the first to report G-to-A hypermutation in a retrovirus, now known to be the result of cytidine deamination by host restriction APOBEC3 proteins. Dr. Pathak became an Assistant Professor in the Department of Biochemistry and the Mary Babb Randolph Cancer Center at West Virginia University in 1991 and was promoted to Associate Professor with tenure in 1998. He joined the National Cancer Institute in 1999 as Senior Investigator and Head of the Viral Mutation Section in the HIV Dynamics and Replication Program (renamed the HIV Dynamics and Replication Program in 2015). He was appointed as Guest Editor for the "HIV Drug Resistance" special issue of Viruses, published in 2010. He received the NIH Asian and Pacific Islander American Organization Award for outstanding accomplishments in biomedical research and an NIH Group Merit Award in 2012 and an NIH Special Act or Service Award in 2020. A research team led by Dr. Pathak received the 2020 Cozzarelli Prize in the Biomedical Sciences class for their PNAS publication “HIV-1 uncoats in the nucleus near sites of integration”; this prize was awarded to just 6 papers chosen from nearly 4,000 published research articles in 2020, recognizing the most outstanding contributions to the scientific disciplines represented by the National Academy of Sciences. Dr. Pathak has also received numerous research funding awards, including a U.S.-Russian Joint Working Group on Biomedical Research Cooperation Award, six NIH Intramural AIDS Targeted Antiviral Program (IATAP) Research Awards, eight IATAP Equipment Awards, two NIH Office of AIDS Research (OAR) Innovation Awards, an OAR Intramural Project Award, and two NIH Bench-to-Bedside Awards. He served as Co-Chair (2013-2014) and Chair (2015) of the Annual Norman P. Salzman Memorial Symposium in Virology, NIH. In 2017, he served as Co-Organizer of the Cold Spring Harbor Laboratory Retroviruses Meeting. He was Co-Organizer of the widely attended NIH/FDA COVID-19 Research Symposium/Workshop in 2020 and is one of six Associate Chairs and the sole NCI member of the NIH-wide COVID-19 Scientific Interest Group Leadership Committee. He also currently serves as a member of the NCI RNA Biology Initiative and the Editorial Boards of Retrovirology, Journal of Virology, and Viruses.
Selected Publications
- Li C, Burdick RC, Nagashima K, Hu WS, Pathak VK. HIV-1 cores retain their integrity until minutes before uncoating in the nucleus. Proc Natl Acad Sci U S A. 2021;118(10).
- Burdick RC, Li C, Munshi M, Rawson JMO, Nagashima K, Hu WS, Pathak VK. HIV-1 uncoats in the nucleus near sites of integration. Proc Natl Acad Sci U S A. 2020;117(10):5486-5493.
- Burdick RC, Delviks-Frankenberry KA, Chen J, Janaka SK, Sastri J, Hu WS, Pathak VK. Dynamics and regulation of nuclear import and nuclear movements of HIV-1 complexes. PLoS Pathog. 2017;13(8):e1006570.
- Delviks-Frankenberry KA, Nikolaitchik OA, Burdick RC, Gorelick RJ, Keele BF, Hu WS, Pathak VK. Minimal Contribution of APOBEC3-Induced G-to-A Hypermutation to HIV-1 Recombination and Genetic Variation. PLoS Pathog. 2016;12(5):e1005646.
- Paprotka T, Delviks-Frankenberry KA, Cingöz O, Martinez A, Kung HJ, Tepper CG, Hu WS, Fivash MJ Jr, Coffin JM, Pathak VK. Recombinant origin of the retrovirus XMRV. Science. 2011;333(6038):97-101.
Related Scientific Focus Areas


Microbiology and Infectious Diseases
View additional Principal Investigators in Microbiology and Infectious Diseases

Molecular Biology and Biochemistry
View additional Principal Investigators in Molecular Biology and Biochemistry

This page was last updated on Saturday, November 22, 2025