Research Topics
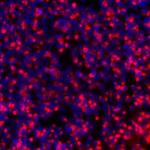
The purpose of our research is to understand the mechanisms of disease and to improve treatment and prevention of hepatitis B virus (HBV) and hepatitis C virus (HCV) infections, and viral hepatitis-associated hepatocellular carcinoma (HCC).
Current Research
Infection with hepatitis B and C viruses affects more than 10 percent of the world population and is the most common etiology of chronic liver disease and hepatocellular carcinoma, which is the fourth leading cause of death from cancer in the world. Current therapies for both viruses are less than optimal. While an effective vaccine for HBV is available, the prospect for a HCV vaccine remains elusive. Given the magnitude and severity of both viral infections as a global public health problem, it is imperative to develop and implement effective prophylactic vaccines and better therapeutic regimens. To achieve this goal, we must understand at the molecular, cellular and genetic levels the viral life cycle, viral mechanisms for productive and persistent infection, virus-host interactions, and host immune responses. The thematic effort of my laboratory focuses on these topics.
While many gaps in our knowledge of HCV exist, great strides have been made in characterizing the virus and functions of viral genes as well as in unraveling the replication pathway and immunologic mechanisms of liver injury. HCV, like many other viruses, exploit host cellular machinery for productive infection. However, unlike other RNA viruses, HCV has a high propensity to cause persistent infection despite an active host immune response. Thus, it possesses unique mechanisms to counteract the various host defenses. HCV gene products have been shown to interact with many host factors and to induce cellular alterations vital for viral replication, persistence and pathogenesis. Earlier progress in HCV research has been hampered by a lack of robust infectious and replicating cell culture systems and convenient small animal models. The development of in vitro systems including infectious cell cultures affords the opportunity to fully characterize viral replication and virus-cell interactions. My lab studies the mechanisms of antivirals in HCV therapy, and to explore the biological basis of treatment non-response in order to improve current treatment regimen. We apply molecular, biochemical and functional genomic tools to identify and characterize structural and functional interactions among the virus, viral gene products, cellular pathways and the host. In addition, we are generating novel reagents and tools for developing and evaluating vaccines and antivirals by building and improving on currently available model systems. Using these technologies, we have developed novel antivirals targeting the entry/fusion process of HCV infection. By applying the technology of induced pluripotent stem cells and hepatocyte differentiation, we have established useful cell model systems to study viral replication and virus-cell interaction. SCID/uPA mice transplanted with human hepatocytes susceptible to HCV infection and transgenic mouse models have been useful as small animal models. Finally, despite the development of highly effective treatments for HCV, we still do not have an effective preventive vaccine. To that end, we are applying molecular, immunological, structural and chemical biology approaches to develop candidate vaccines.
For HBV, the replication and virus-host interactions have been studied in great details and many of the pathways have been elucidated. The availability of culture systems and small animal models has greatly facilitated the elucidation of fundamental knowledge of the virus and the evaluation of vaccine and therapeutic candidates. While the various virological functions in replication are well-known, the roles of interacting cellular factors remain largely undefined. In addition, the viral and host functions for productive and persistent infection in vivo are poorly understood. Among the viral gene products, the accessory proteins HBeAg and HBX are not essential for replication in vitro but appear to be important for viral infection in vivo. The HBX has multifarious effects and appears to function through several pathways including signal transduction, transcriptional activation/DNA repair, and/or cellular proteolysis. These mechanisms may not be mutually exclusive and can be concurrently operative in contributing to the pleiotropic effect of HBX. Despite the uncertainty about the mechanism of HBX functions, it has been generally accepted that this gene product is required for the establishment of HBV infection in vivo. We have been focusing on understanding the functions of HBX and developing therapeutic strategy targeting at this important viral function. We have established various infectious HBV cell culture systems that are suitable to study HBV infection, spread, virus-cell interaction and antiviral testing. We are also applying a similar overall approach in functional genomics and genome-wide screens described above for HCV to studying HBV-host interactions.
Building on our extensive experiences in antiviral development, we have also established an active research program on therapeutic development of COVID-19, with focus on the entry/fusion process of infection.
Finally, we have established an active research program on the increasingly important problem of hepatocellular carcinoma in the context of chronic viral hepatitis. We are developing various in vitro and in vivo models to identify and study potentially important pro-carcinogenic pathways that are triggered by HBV or HCV infection. By leveraging this knowledge, we hope to uncover novel strategies for preventive and therapeutic interventions of this deadly cancer.
Biography
- American Academy of Microbiology, 2018
- National Academy of Medicine, 2016
- Association of American Physicians, 2002
- American Society for Clinical Investigation, 1996
- Elected Fellow of the AAAS, American Association for the Study of Liver Diseases, & American Gastroenterological Association
- Gastroenterology & Hepatology Fellowship, Massachusetts General Hospital & Harvard Medical School, 1987-1990
- Internal Medicine Residency, New York University & Bellevue Hospital, 1984-1987
- M.D., Harvard Medical School, 1984
- B.A., Harvard College, 1980
Selected Publications
- Liang TJ, Feld JJ, Cox AL, Rice CM. Controlled Human Infection Model - Fast Track to HCV Vaccine? N Engl J Med. 2021;385(13):1235-1240.
- Zhang M, Zhang Z, Imamura M, Osawa M, Teraoka Y, Piotrowski J, Ishida Y, Sozzi V, Revill PA, Saito T, Chayama K, Liang TJ. Infection courses, virological features and IFN-α responses of HBV genotypes in cell culture and animal models. J Hepatol. 2021;75(6):1335-1345.
- Xia Y, Cheng X, Nilsson T, Zhang M, Zhao G, Inuzuka T, Teng Y, Li Y, Anderson DE, Holdorf M, Liang TJ. Nucleolin binds to and regulates transcription of hepatitis B virus covalently closed circular DNA minichromosome. Proc Natl Acad Sci U S A. 2023;120(49):e2306390120.
- Cheng X, Uchida T, Xia Y, Umarova R, Liu CJ, Chen PJ, Gaggar A, Suri V, Mücke MM, Vermehren J, Zeuzem S, Teraoka Y, Osawa M, Aikata H, Tsuji K, Mori N, Hige S, Karino Y, Imamura M, Chayama K, Liang TJ. Diminished hepatic IFN response following HCV clearance triggers HBV reactivation in coinfection. J Clin Invest. 2020;130(6):3205-3220.
- Hu Z, Rolt A, Hu X, Ma CD, Le DJ, Park SB, Houghton M, Southall N, Anderson DE, Talley DC, Lloyd JR, Marugan JC, Liang TJ. Chlorcyclizine Inhibits Viral Fusion of Hepatitis C Virus Entry by Directly Targeting HCV Envelope Glycoprotein 1. Cell Chem Biol. 2020;27(7):780-792.e5.
Related Scientific Focus Areas
This page was last updated on Thursday, August 7, 2025