
Sarah Elizabeth Sheppard, M.D.,M.S.,Ph.D.
Investigator
Unit on Vascular Malformations
NICHD/DIR
Research Topics
The primary goal of Dr. Sheppard’s translational research group is to develop more efficacious therapies for patients with malformations of the lymphatic system. Specifically, her research has focused on a subtype of complex lymphatic anomaly, called central conducting lymphatic anomaly (also known as channel type lymphatic malformation), with severe morbidity and mortality.
Central conducting lymphatic anomalies (CCLA) occur when there is a disruption of central lymphatic flow resulting in complications such as non-immune fetal hydrops, chylothorax, chylous ascites, protein-losing enteropathy, other effusions, or lymphedema. The heterogeneity of CCLA complicates diagnosis, treatment, and prognostication. Additionally, only about 25% of patients with this disorder have an underlying genetic diagnosis that can be identified. Research from Dr. Sheppard and collaborators identified multiple genetic causes of CCLA and showed that germline RASopathies, mosaic KRASopathies, PIEZO1-related lymphatic dysplasia, and Trisomy 21 all have distinct central lymphatic flow phenotypes. Dr. Sheppard and collaborators also demonstrated that pathogenic mosaic activating variants in KRAS cause CCLA which respond to MEK inhibition in both organoid and zebrafish models.
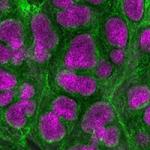
In her group at NICHD, Dr. Sheppard’s translational research program will have multiple arms. The wet laboratory will elucidate the cellular and molecular mechanisms for known and novel genetic causes of CCLA using organoids and the zebrafish. New therapies will be identified using a drug repurposing strategy. The clinical arm will initially focus on a natural history study for patients with CCLA to understand the disease. This will assist in more efficacious and precise endpoints to study in future clinical trials. A secondary outcome of the natural history study will be to improve molecular diagnosis in patients with CCLA. Eventually, the group will conduct clinical trials from the drugs identified in the laboratory.
Biography
Sarah Sheppard is a clinical tenure-track investigator at NICHD and a 2021 NIH Distinguished Scholar. She graduated from the Massachusetts Institute of Technology with a bachelors of science in Nuclear Science and Engineering. She attained her medical degree and doctorate through a combined MD PhD program at the University of Massachusetts Medical School. During her doctorate, Dr. Sheppard studied post-transcriptional regulation of vascular development in the zebrafish in the laboratory of Dr. Nathan Lawson. She then completed her combined pediatrics and clinical genetics residency at the Children’s Hospital of Philadelphia (CHOP). Following her clinical training, she practiced as a clinical geneticist in Division of Human Genetics, the Comprehensive Vascular Anomaly Program, and the Jill and Mark Fishman Lymphatic Center at CHOP. She completed a Masters of Translational Research at the Perelman School of Medicine at the University of Pennsylvania and post-doctoral fellowship with Dr. Hakon Hakonarson in the Center of Applied Genomics at CHOP. Her post-doctoral work focused on improving diagnosis and treatment for patients with a type of lymphatic disorder called central conducting lymphatic anomaly. Her accolades include the Children’s Hospital of Philadelphia Distinguished Research Trainee Award (2019) and the Association for Clinical and Translational Sciences Outstanding Post-Doctoral Trainee Award (2020). In addition to the NIH, her research has been funded by the American Heart Association, the American Society of Transplant Surgeons, the Institute of Translational Medicine and Therapeutics at the University of Pennsylvania, the Children’s Hospital of Philadelphia, Uplifting Athletes, and the Lymphangiomatosis and Gorham’s Disease Alliance.
Selected Publications
- Li D, Sheppard SE, March ME, Battig MR, Surrey LF, Srinivasan AS, Matsuoka LS, Tian L, Wang F, Seiler C, Dayneka J, Borst AJ, Matos MC, Paulissen SM, Krishnamurthy G, Nriagu B, Sikder T, Casey M, Williams L, Rangu S, O'Connor N, Thomas A, Pinto E, Hou C, Nguyen K, Pellegrino da Silva R, Chehimi SN, Kao C, Biroc L, Britt AD, Queenan M, Reid JR, Napoli JA, Low DM, Vatsky S, Treat J, Smith CL, Cahill AM, Snyder KM, Adams DM, Dori Y, Hakonarson H. Genomic profiling informs diagnoses and treatment in vascular anomalies. Nat Med. 2023;29(6):1530-1539.
- Sheppard SE, March ME, Seiler C, Matsuoka LS, Kim SE, Kao C, Rubin AI, Battig MR, Khalek N, Schindewolf E, O'Connor N, Pinto E, Priestley JR, Sanders VR, Niazi R, Ganguly A, Hou C, Slater D, Frieden IJ, Huynh T, Shieh JT, Krantz ID, Guerrero JC, Surrey LF, Biko DM, Laje P, Castelo-Soccio L, Nakano TA, Snyder K, Smith CL, Li D, Dori Y, Hakonarson H. Lymphatic disorders caused by mosaic, activating KRAS variants respond to MEK inhibition. JCI Insight. 2023;8(9).
- Liu M, Smith CL, Biko DM, Li D, Pinto E, O'Connor N, Skraban C, Zackai EH, Hakonarson H, Dori Y, Sheppard SE. Genetics etiologies and genotype phenotype correlations in a cohort of individuals with central conducting lymphatic anomaly. Eur J Hum Genet. 2022;30(9):1022-1028.
- Garlisi Torales LD, Sempowski BA, Krikorian GL, Woodis KM, Paulissen SM, Smith CL, Sheppard SE. Central conducting lymphatic anomaly: from bench to bedside. J Clin Invest. 2024;134(8).
- Szigety KM, Crowley TB, Gaiser KB, Chen EY, Priestley JRC, Williams LS, Rangu SA, Wright CM, Adusumalli P, Ahrens-Nicklas RC, Calderon B, Cuddapah SR, Edmondson A, Ficicioglu C, Ganetzky R, Kalish JM, Krantz ID, McDonald-McGinn DM, Medne L, Muraresku C, Pyle LC, Zackai EH, Campbell IM, Sheppard SE. Clinical Effectiveness of Telemedicine-Based Pediatric Genetics Care. Pediatrics. 2022;150(1).
Related Scientific Focus Areas


Molecular Biology and Biochemistry
View additional Principal Investigators in Molecular Biology and Biochemistry
This page was last updated on Tuesday, January 3, 2023