
Research Topics
The aim of the Cellular Immunology Section (CIS) is to provide a mechanistic basis for developing preventive vaccines against HIV, malaria, tuberculosis, SARS-CoV2 and therapeutic vaccines against cancer. More recently, there is a major focus on developing monoclonal antibodies against proteins expressed on malaria parasites to be used as passive prevention.
T cell Immunity: Based on the critical role of CD4 and CD8 T cells in mediating protection against infections and tumors, a major area of investigation is to understand how various vaccine platforms influence the magnitude, quality, breadth and tissue distribution following immunization. T-cell responses are assessed with a variety of technologies including advanced 30-color multi-parameter flow cytometry, single cell analysis by RNAseq, spatial transcriptomics and confocal imaging.
Innate Immunity: The laboratory has a major focus on determining how different immune adjuvants, formulation and delivery influence humoral and cellular immunity when administered with protein or peptide antigens specific for viral infections or cancer antigens. Recent work has focused on using polymer chemistry and other bio-engineering approaches with specific toll-like receptor (TLR) ligands (eg. TLR 7/8) or STING to tumor specific neo-antigen responses to be used for personalized cancer vaccines.
Vaccines: The laboratory has focused on vaccines against HIV, TB, malaria, cancer and more recently SARS-CoV2. These studies focus on using different vaccine formulations such as protein/adjuvant, viral vectors or synthetic nanoparticle vaccines alone or in heterologous prime boost combinations. There is a major emphasis on how the route of immunization influences antibody and T cell responses in tissues such as lung and liver which are important for mediating protection against respiratory infection or malaria respectively.
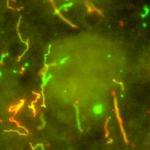
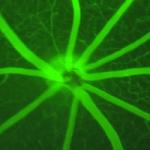
Malaria Monoclonal Antibodies: The laboratory has isolated a large number of human monoclonal antibodies against the major circumsporozoite surface protein expressed on P. falciparum sporozoites (PfCSP). The specificity and function of such antibodies binding to PfCSP are elucidated by epitope mapping, avidity and stoichiometry measurements and defining the crystal structure. in vivo imaging is used to understand the mechanism of how the antibodies mediate protection in the skin and liver.
Clinical Translation: 1) Malaria-Based on the discovery that intravenous immunization with an attenuated sporozoite vaccine induced a high frequency of tissue resident T cells in the liver in pre-clinical animal models, Dr. Seder has led several clinical trials in the US and Africa with an attenuated sporozoite vaccine given by the intravenous route for safety and clinical efficacy. In addition, Dr. Seder has recently performed the first in human clinical trial showing that a monoclonal antibody can prevent malaria infection in humans. This has led to several ongoing and planned trials to use monoclonal antibodies to prevent malaria infection in infants and children in Africa. 2) Personalized tumor vaccine- Based on the discovery/development of a personalized neoantigen peptide/adjuvant nanoparticle vaccine in pre-clinical models, there are plans for assessing this in human clinical trials.
Biography
Dr. Seder received his B.A. in Natural Science at Johns Hopkins University in 1981 and his M.D. at Tufts University in 1986 and completed his residency in internal medicine at New York Hospital-Cornell Medical Center. Dr. Seder did his postdoctoral training at NIAID with Dr. William Paul. He is currently Chief of the Cellular Immunology Section in the Vaccine Research Center in the NIAID, NIH. Dr. Seder's laboratory has focused on the cellular and molecular mechanisms by which vaccines and adjuvants mediate protective immunity in mouse, and non-human primate models of HIV, Malaria, Tuberculosis and cancer. His work has demonstrated the importance of the quality of T cell responses in mediating protection against various infections and the importance of the route of vaccination in generating tissue resident T cells for protection against malaria and TB. Dr. Seder has translated his scientific discoveries and led the first in human clinical studies using intravenous vaccination to generate protective immunity with an attenuated malaria vaccine and recently showed that a monoclonal antibody he discovered can prevent malaria infection against intense seasonal transmission in African adults. Over the two years, Dr. Seder has helped lead the pre-clinical development of the Moderna mRNA vaccine against COVID. This provided pre-clinical data for demonstrating safety and efficacy of the Moderna vaccine in animals prior to the initiation of the pivotal Phase 3 study in humans and more recently provided the scientific basis for boosting humans with mRNA against variants.
Selected Publications
- Darrah PA, Zeppa JJ, Maiello P, Hackney JA, Wadsworth MH 2nd, Hughes TK, Pokkali S, Swanson PA 2nd, Grant NL, Rodgers MA, Kamath M, Causgrove CM, Laddy DJ, Bonavia A, Casimiro D, Lin PL, Klein E, White AG, Scanga CA, Shalek AK, Roederer M, Flynn JL, Seder RA. Prevention of tuberculosis in macaques after intravenous BCG immunization. Nature. 2020;577(7788):95-102.
- Corbett KS, Flynn B, Foulds KE, Francica JR, Boyoglu-Barnum S, Werner AP, Flach B, O'Connell S, Bock KW, Minai M, Nagata BM, Andersen H, Martinez DR, Noe AT, Douek N, Donaldson MM, Nji NN, Alvarado GS, Edwards DK, Flebbe DR, Lamb E, Doria-Rose NA, Lin BC, Louder MK, O'Dell S, Schmidt SD, Phung E, Chang LA, Yap C, Todd JM, Pessaint L, Van Ry A, Browne S, Greenhouse J, Putman-Taylor T, Strasbaugh A, Campbell TA, Cook A, Dodson A, Steingrebe K, Shi W, Zhang Y, Abiona OM, Wang L, Pegu A, Yang ES, Leung K, Zhou T, Teng IT, Widge A, Gordon I, Novik L, Gillespie RA, Loomis RJ, Moliva JI, Stewart-Jones G, Himansu S, Kong WP, Nason MC, Morabito KM, Ruckwardt TJ, Ledgerwood JE, Gaudinski MR, Kwong PD, Mascola JR, Carfi A, Lewis MG, Baric RS, McDermott A, Moore IN, Sullivan NJ, Roederer M, Seder RA, Graham BS. Evaluation of the mRNA-1273 Vaccine against SARS-CoV-2 in Nonhuman Primates. N Engl J Med. 2020;383(16):1544-1555.
- Gagne M, Moliva JI, Foulds KE, Andrew SF, Flynn BJ, Werner AP, Wagner DA, Teng IT, Lin BC, Moore C, Jean-Baptiste N, Carroll R, Foster SL, Patel M, Ellis M, Edara VV, Maldonado NV, Minai M, McCormick L, Honeycutt CC, Nagata BM, Bock KW, Dulan CNM, Cordon J, Flebbe DR, Todd JM, McCarthy E, Pessaint L, Van Ry A, Narvaez B, Valentin D, Cook A, Dodson A, Steingrebe K, Nurmukhambetova ST, Godbole S, Henry AR, Laboune F, Roberts-Torres J, Lorang CG, Amin S, Trost J, Naisan M, Basappa M, Willis J, Wang L, Shi W, Doria-Rose NA, Zhang Y, Yang ES, Leung K, O'Dell S, Schmidt SD, Olia AS, Liu C, Harris DR, Chuang GY, Stewart-Jones G, Renzi I, Lai YT, Malinowski A, Wu K, Mascola JR, Carfi A, Kwong PD, Edwards DK, Lewis MG, Andersen H, Corbett KS, Nason MC, McDermott AB, Suthar MS, Moore IN, Roederer M, Sullivan NJ, Douek DC, Seder RA. mRNA-1273 or mRNA-Omicron boost in vaccinated macaques elicits similar B cell expansion, neutralizing responses, and protection from Omicron. Cell. 2022;185(9):1556-1571.e18.
- Baharom F, Ramirez-Valdez RA, Khalilnezhad A, Khalilnezhad S, Dillon M, Hermans D, Fussell S, Tobin KKS, Dutertre CA, Lynn GM, Müller S, Ginhoux F, Ishizuka AS, Seder RA. Systemic vaccination induces CD8(+) T cells and remodels the tumor microenvironment. Cell. 2022;185(23):4317-4332.e15.
- Wu RL, Idris AH, Berkowitz NM, Happe M, Gaudinski MR, Buettner C, Strom L, Awan SF, Holman LA, Mendoza F, Gordon IJ, Hu Z, Campos Chagas A, Wang LT, Da Silva Pereira L, Francica JR, Kisalu NK, Flynn BJ, Shi W, Kong WP, O'Connell S, Plummer SH, Beck A, McDermott A, Narpala SR, Serebryannyy L, Castro M, Silva R, Imam M, Pittman I, Hickman SP, McDougal AJ, Lukoskie AE, Murphy JR, Gall JG, Carlton K, Morgan P, Seo E, Stein JA, Vazquez S, Telscher S, Capparelli EV, Coates EE, Mascola JR, Ledgerwood JE, Dropulic LK, Seder RA, VRC 614 Study Team. Low-Dose Subcutaneous or Intravenous Monoclonal Antibody to Prevent Malaria. N Engl J Med. 2022;387(5):397-407.
Related Scientific Focus Areas

Microbiology and Infectious Diseases
View additional Principal Investigators in Microbiology and Infectious Diseases

This page was last updated on Tuesday, December 6, 2022