Research Topics
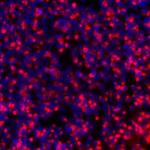
As tenured investigator in the NHLBI, Dr. Childs has focused his research on allogeneic stem cell transplantation and tumor immunology to treat aplastic anemia, hematological malignancies, and solid tumors. Dr. Childs and his research team were the first to establish the existence of a graft-vs-solid tumor effect mediated by transplanted donor T-cells that could cure patients with metastatic renal cell carcinoma. Subsequently, his laboratory discovered a novel human endogenous retrovirus (HERV-E) to be the target for allogeneic graft-vs-tumor effects inducing tumor regression. Translational research being conducted in his lab is focused on developing novel T-cell based approaches to target HERV-E derived kidney cancer antigens in clear cell renal cell carcinoma. In this regard, his group has cloned T-cell receptors recognizing HERV-E antigens and in a first in human clinical trial being conducted at the NIH Clinical Center, is investigating the anti-tumor potential of adoptively transferring autologous T-cells genetically modified to express HERV-E T-cell receptors. Dr. Childs’ lab also has a major focus on NK Cell immunotherapy, conducting lab based and clinical research aimed at exploring a variety of different strategies to optimize adoptive NK cell therapy for cancer. Dr. Childs also serves as the principal investigator on several investigator-initiated clinical research protocols conducted at the NIH Clinical Center exploring novel hematopoietic stem cell transplant regimens aimed at improving transplant-outcomes for patients with treatment refractory severe aplastic anemia, and has performed over 400 hundred experimental stem cell transplants at the NHLBI.
Biography
Rear Admiral (RADM) Richard Childs serves as the Scientific Director of the National Heart, Lung, and Blood Institute (NHLBI) at the National Institutes of Health (NIH). He graduated from Georgetown University and Georgetown University Medical School. He completed his internship, residency, and a Chief Residency in internal medicine at the University of Florida in Gainesville followed by fellowships in Medical Oncology at the National Cancer Institute (NCI), NIH, and Hematology at the NHLBI, NIH. Following fellowship training, he was appointed a tenure-track investigator in the Hematology Branch of the NHLBI and received tenure at the NIH in 2006. He was the first investigator to show that metastatic kidney cancer could be cured by transplanted allogeneic immune cells through a graft-vs-tumor effect, a seminal discovery that was published in the New England Journal of Medicine. He continues to run a translational research lab that conducts first-in-human research in bone marrow transplantation and tumor immunotherapy. He is board certified in medical oncology, has performed more than 600 experimental bone marrow stem cell transplants at the NIH, holds more than 30 patents related to NK and T-cell based immunotherapy, and has published over 240 original research papers as the lead or senior author.
In his previous role as NHLBI Clinical Director, he directed one of the NIH’s largest clinical and translational science programs, having oversight of all of the NHLBI’s intramural research in heart, lung, and blood diseases, which includes over 250 investigator-initiated clinical trials. As Clinical Director, he spearheaded and operationalized a multi-million dollar strategic plan in 2015 that completely revamped his institute’s research infrastructure, revitalizing NHLBI’s clinical research enterprise which substantially improved and expanded its clinical research footprint and productivity.
Dr. Childs has been an active duty officer in the United Stated Commissioned Corps since 1995. He was promoted to Rear Admiral in 2015 and in 2020 received his 2nd star, and currently serves as an Assistant United States Surgeon General. In 2014, he deployed to Liberia, West Africa, as a part of the United States Ebola Crisis Response, where he served as the Chief Medical Officer caring for Ebola patients in the Monrovia Medical Unit (MMU). In 2020, he commanded a rapid response deployment team to Yokohama, Japan, that evacuated hundreds of COVID-19 infected/exposed Americans from the Diamond Princess cruise ship and provided compassionate use remdesivir for severe and critically ill passengers suffering with severe COVID-19, well before this drug received approval as a treatment for SARS-CoV-2. These actions earned him the United States Meritorious Service Medal, the Distinguished Service Medal with Valor, the Humanitarian Service and Global Health Award, and the Assistant Secretary of Health’s Exceptional Service Medal.
Selected Publications
- Barisic S, Brahmbhatt EM, Cherkasova E, Spear TT, Savani U, Pierre S, Scurti GM, Chen L, Igboko M, Nadal R, Zeng G, Parry G, Stroncek DF, Highfill S, Dalheim AV, Reger R, Nishimura MI, Childs RW. Regression of renal cell carcinoma by T cell receptor-engineered T cells targeting a human endogenous retrovirus. J Immunother Cancer. 2024;12(9).
- Takahashi Y, Harashima N, Kajigaya S, Yokoyama H, Cherkasova E, McCoy JP, Hanada K, Mena O, Kurlander R, Tawab A, Srinivasan R, Lundqvist A, Malinzak E, Geller N, Lerman MI, Childs RW. Regression of human kidney cancer following allogeneic stem cell transplantation is associated with recognition of an HERV-E antigen by T cells. J Clin Invest. 2008;118(3):1099-109.
- Cherkasova E, Scrivani C, Doh S, Weisman Q, Takahashi Y, Harashima N, Yokoyama H, Srinivasan R, Linehan WM, Lerman MI, Childs RW. Detection of an Immunogenic HERV-E Envelope with Selective Expression in Clear Cell Kidney Cancer. Cancer Res. 2016;76(8):2177-85.
- Chanswangphuwana C, Allan DSJ, Chakraborty M, Reger RN, Childs RW. Augmentation of NK Cell Proliferation and Anti-tumor Immunity by Transgenic Expression of Receptors for EPO or TPO. Mol Ther. 2021;29(1):47-59.
- Childs R, Chernoff A, Contentin N, Bahceci E, Schrump D, Leitman S, Read EJ, Tisdale J, Dunbar C, Linehan WM, Young NS, Barrett AJ. Regression of metastatic renal-cell carcinoma after nonmyeloablative allogeneic peripheral-blood stem-cell transplantation. N Engl J Med. 2000;343(11):750-8.
Related Scientific Focus Areas
This page was last updated on Wednesday, September 3, 2025