Peter Grayson, M.D., M.Sc.
Senior Investigator
Vasculitis Translational Research Program
NIAMS
Research Topics
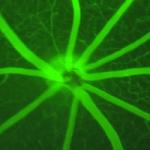
Dr. Grayson's research focuses on clinical and translational research across many forms of systemic vasculitis. Specifically, his work has focused on biomarker discovery/development, advanced molecular imaging, molecular classification of disease, clinical trials, and genetics/genomics of vasculitis. His group co-discovered the VEXAS syndrome in 2020. His group has clinically defined advanced molecular imaging as a surrogate marker of vascular inflammation in large-vessel vasculitis.
His group has conducted some of the only translational work related to relapsing polychondritis, including identifying somatic mutations in UBA1 as a driver of disease in a subset of these patients. Translational work from the group has also defined novel pathways of neutrophil-mediated inflammation in monogenic vasculitis and drug-induced vasculitis and has identified novel biomarkers of disease activity in many forms of vasculitis that suggest novel therapeutic targets.
Biography
Peter Grayson, M.D., M.Sc., is a senior investigator at the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS). He completed his undergraduate degree from Brown University in 1999, his medical degree from the Medical University of South Carolina in 2004, and his master's in science from Boston University in 2008. He served as a chief resident in Internal Medicine at Boston Medical Center and completed an additional two-year vasculitis fellowship within the Vasculitis Clinical Research Consortium.
Dr. Grayson is firmly committed to mentoring young investigators in rare disease research. He served as the acting program director for the NIAMS Rheumatology Fellowship Program and is the recipient of numerous teaching awards. He received the American College of Rheumatology's Distinguished Fellow Award in 2011 and was elected into the American Society for Clinical Investigation in 2024.
Selected Publications
- Beck DB, Ferrada MA, Sikora KA, Ombrello AK, Collins JC, Pei W, Balanda N, Ross DL, Ospina Cardona D, Wu Z, Patel B, Manthiram K, Groarke EM, Gutierrez-Rodrigues F, Hoffmann P, Rosenzweig S, Nakabo S, Dillon LW, Hourigan CS, Tsai WL, Gupta S, Carmona-Rivera C, Asmar AJ, Xu L, Oda H, Goodspeed W, Barron KS, Nehrebecky M, Jones A, Laird RS, Deuitch N, Rowczenio D, Rominger E, Wells KV, Lee CR, Wang W, Trick M, Mullikin J, Wigerblad G, Brooks S, Dell'Orso S, Deng Z, Chae JJ, Dulau-Florea A, Malicdan MCV, Novacic D, Colbert RA, Kaplan MJ, Gadina M, Savic S, Lachmann HJ, Abu-Asab M, Solomon BD, Retterer K, Gahl WA, Burgess SM, Aksentijevich I, Young NS, Calvo KR, Werner A, Kastner DL, Grayson PC. Somatic Mutations in UBA1 and Severe Adult-Onset Autoinflammatory Disease. N Engl J Med. 2020;383(27):2628-2638.
- Grayson PC, Alehashemi S, Bagheri AA, Civelek AC, Cupps TR, Kaplan MJ, Malayeri AA, Merkel PA, Novakovich E, Bluemke DA, Ahlman MA. (18) F-Fluorodeoxyglucose-Positron Emission Tomography As an Imaging Biomarker in a Prospective, Longitudinal Cohort of Patients With Large Vessel Vasculitis. Arthritis Rheumatol. 2018;70(3):439-449.
- Carmona-Rivera C, Purmalek MM, Moore E, Waldman M, Walter PJ, Garraffo HM, Phillips KA, Preston KL, Graf J, Kaplan MJ, Grayson PC. A role for muscarinic receptors in neutrophil extracellular trap formation and levamisole-induced autoimmunity. JCI Insight. 2017;2(3):e89780.
- Carmona-Rivera C, Khaznadar SS, Shwin KW, Irizarry-Caro JA, O'Neil LJ, Liu Y, Jacobson KA, Ombrello AK, Stone DL, Tsai WL, Kastner DL, Aksentijevich I, Kaplan MJ, Grayson PC. Deficiency of adenosine deaminase 2 triggers adenosine-mediated NETosis and TNF production in patients with DADA2. Blood. 2019;134(4):395-406.
- Ferrada MA, Savic S, Cardona DO, Collins JC, Alessi H, Gutierrez-Rodrigues F, Kumar DBU, Wilson L, Goodspeed W, Topilow JS, Paik JJ, Poulter JA, Kermani TA, Koster MJ, Warrington KJ, Cargo C, Tattersall RS, Duncan CJA, Cantor A, Hoffmann P, Payne EM, Bonnekoh H, Krause K, Cowen EW, Calvo KR, Patel BA, Ombrello AK, Kastner DL, Young NS, Werner A, Grayson PC, Beck DB. Translation of cytoplasmic UBA1 contributes to VEXAS syndrome pathogenesis. Blood. 2022;140(13):1496-1506.
Related Scientific Focus Areas
This page was last updated on Tuesday, November 12, 2024