Research Topics
During the next few years, our new group in the Pediatric Oncology Branch aims to combine fundamental and translational approaches to respond to key questions addressing the metabolic regulation of T cell effector function and hematopoietic stem cell (HSC) differentiation in pediatric cancer patients and develop intrathymic-based strategies that enhance thymocyte differentiation and T cell function.
Specific projects focus on:
Role of the microenvironment on T cell effector function and anti-tumor immunotherapy
Despite many advances in anti-cancer therapies, metastatic cancers remain difficult to treat. In this context, new approaches are being developed, such as adoptive immunotherapies that aim to modify the balance between tumor-specific immune cells and cancer cells. While immunotherapy strategies have clearly demonstrated their promising potential, it is critical that we optimize the persistence and responsiveness of adoptively transferred T cells. One issue is that the ability of immune cells in general, and T cells in particular, to respond to tumor antigens is often negatively modulated by the metabolic environment of the tumor. We are therefore interested in elucidating the metabolic characteristics that promote an optimal anti-tumor T cell response, as a function of the T cell differentiation state and in the “hostile” tumor tissue that consumes high levels of nutrients and is often anaerobic. Furthermore, we will focus on understanding the impact of a patient’s chemotherapy regimen on the metabolic fitness of an effector T cell in the tumor environment.
Conditioning hematopoietic stem cell differentiation via nutrient transporters and metabolite fluxes
HSCs are defined by their self-renewal and multi-lineage differentiation potential, allowing them to provide long-term reconstitution of all blood lineages. During the past two decades, extensive research has been aimed at elucidating the roles of cytokines and the microenvironment in differentiation. However, it is only in the past few years that we have recognized the importance of nutrient resources and hence the regulation of nutrient transporters as critical for the survival and proliferation of hematopoietic stem cells, progenitors and more mature lineage-committed cells. Indeed, it is now accepted that metabolism regulates HSC “stemness”. Our previous studies highlighted the importance of nutrient transport and utilization as regulators of HSC commitment and our future work will focus on the functions of nutrient transporters and downstream metabolite fluxes in directing HSC maintenance and differentiation.
Improving T cell differentiation following HSC transplantation by thymus-targeting and reconstitution strategies
HSC transplantation is almost always performed by the intravenous administration of autologous or allogeneic HSCs. In the context of T cell differentiation, it is presumed that the injected progenitors first home to the bone marrow and those cells that are capable of settling the thymus then migrate, from the bone marrow into the thymus. The kinetics of this migration as well as the length of time during which progenitors continue to enter into the thymus following transplant is still the subject of intense research efforts. Studies from our group and others have shown that the direct intrathymic injection of progenitors promotes a more rapid and robust thymopoiesis, requiring less input HSCs, than following IV HSC administration, even across histocompatibility barriers. This research lays the groundwork for our future studies aimed at developing thymic-based strategies, targeting both hematopoietic progenitors and the diverse thymic stromal environment, with the goal of enhancing T cell regeneration and function following HSC transplantation.
Interested in working with us?
We are always interested in hearing from motivated and interested students and colleagues!
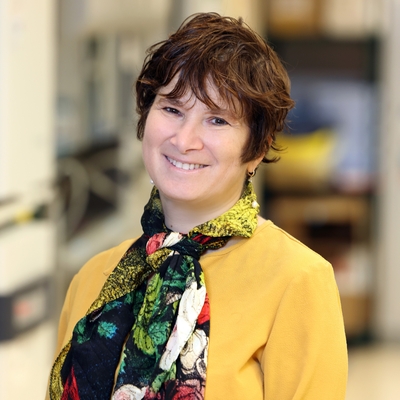
Biography
Naomi Taylor received her M.D. and Ph.D. degrees from Yale University, studying the disruption of Epstein-Barr virus (EBV) latency under the direction of Dr. George Miller. She then returned to clinical pediatrics, pursuing training in bone marrow transplantation at Children's Hospital of Los Angeles. In 1996, Dr. Taylor began her own group at the Institut de Génétique Moléculaire de Montpellier, a joint CNRS/University of Montpellier research institute in the south of France. Her group focused on contributing to our understanding of T cell immunodeficiencies, the development of hematopoietic stem cell and T cell-based therapeutic strategies, and the impact of nutrient transport and utilization in erythropoiesis and lymphopoeisis. She was promoted to a 1st class INSERM Research Director position in 2008 and benefited from two sabbaticals in the Experimental Immunology Branch, National Cancer Institute. In 2018, Dr. Taylor returned to the United States as a Senior Investigator in the Pediatric Oncology Branch, National Cancer Institute. Dr. Taylor remains a visiting Professor at the University of Montpellier.
Related Scientific Focus Areas
This page was last updated on Friday, May 23, 2025