
Research Topics
Since the 1990s, fungal infections have emerged as a major cause of morbidity and mortality in immunosuppressed and critically ill patients. The yeast Candida is the most common human fungal pathogen and is responsible for both invasive and mucosal infections. Neutrophils and monocytes/macrophages are critical for host defense against invasive candidiasis, the most common deep-seated human mycosis and the fourth-leading cause of nosocomial bloodstream infection in the United States. Despite administration of antifungal therapy, mortality of patients who develop invasive Candida infection exceeds 40 percent. In stark contrast to the requirement of phagocytes for defense against invasive infection, mucosal candidiasis develops 1) in patients with impaired cellular immunity such as those with AIDS (more than 90 percent of whom develop oral thrush) or inborn errors of immunity leading to chronic mucocutaneous candidiasis (CMC) and 2) in the majority of healthy women, often associated with antibiotic use (vaginal candidiasis). Invasive aspergillosis, most often caused by the ubiquitous inhaled mold Aspergillus fumigatus, is a leading cause of infection-related mortality in cancer or hematopoietic stem cell transplant (HSCT) patients (mortality, >25-50%) and in patients with chronic granulomatous disease (CGD), who have a defective phagocyte oxidative burst. In all of these conditions, detailed knowledge of immunopathogenesis at the molecular and cellular levels is lacking and could inspire new treatment and prevention approaches.
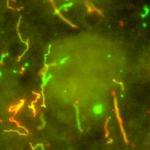
Our laboratory research focuses on 1) cellular and molecular factors that regulate the immune response against mucosal and invasive candidiasis and invasive aspergillosis in clinically relevant animal models and on 2) better understanding the genetic and immune defects that underlie enhanced susceptibility to mucocutaneous and invasive fungal infections in humans. Our goal is to develop a detailed mechanistic understanding of the molecular and cellular basis of innate and adaptive immune responses against Candida and Aspergillus with an aim to devise novel strategies to improve the diagnosis and augment or supplement the current antifungal drug treatment against candidiasis. To this end, we utilize in vitro cell culture systems and clinically relevant mouse models of mucosal and systemic Candida and Aspergillus infections to study host-fungal interactions by using a variety of immunological, biological, and imaging approaches.
The first step in mounting any immune response is the effective recruitment and activation of immune cells at the site of infection. Yet, the molecular factors that mediate these processes in the setting of candidiasis are poorly defined. Hence, a major focus of the laboratory is to investigate the role of specific members of the chemoattractant system in mediating trafficking and effector function of specific resident and recruited immune cells in anti-Candida host defense in vivo. Characterization of the role of Candidate chemotactic factors in antifungal host defense in mice is then followed by human immunogenomics studies, in which genetic polymorphisms in the identified chemotactic factor genes are tested for correlating effects on biological function and for associations with candidiasis in patients.
Further, an important event that determines the outcome of candidiasis is germination of Candida yeast into hyphae. Hence, Candida mutant strains that are unable to germinate are avirulent in vivo. We have previously demonstrated that in disseminated candidiasis, the innate antifungal immune response is highly idiosyncratic for each infected organ, associated with organ-specific differential ability of Candida to filament in these tissues. Thus, our laboratory is interested in delineating the host factors that govern antifungal resistance versus susceptibility at different anatomical sites. To that end, a major focus of our laboratory is the study of the immunological mechanisms that account for central nervous system (CNS)-targeted susceptibility to systemic candidiasis and other systemic fungal infections in patients with CARD9 mutations. Hence, via an investigational review board (IRB)-approved clinical protocol, our lab is recruiting patients with biallelic CARD9 mutations to NIH to study them immunologically. In parallel, the cellular and molecular basis of enhanced susceptibility to CNS-targeted system fungal diseases in CARD9 deficiency is investigated in Card9-/- mice.
With regard to mucosal candidiasis, the laboratory investigates the mechanisms of Candida susceptibility in inherited immunodeficiencies that lead to CMC and in healthy subjects following antibiotic use. Hence, the laboratory aims to define the immunological mechanisms that account for universal susceptibility to CMC in patients with the autosomal-recessive autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy (APECED) syndrome. APECED, caused by mutations in autoimmune regulator (AIRE), is the only primary immunodeficiency in which CMC develops in >90 percent of patients and is the only consistent infectious disease phenotype. Hence, our laboratory, via an investigational review board (IRB)-approved clinical protocol, has recruited ~200 APECED patients to the National Institutes of Health to study them immunologically. In parallel, the cellular and molecular basis of enhanced susceptibility to mucosal candidiasis in APECED is investigated in Aire-/- mice. In addition to investigating mechanisms of CARD9-dependent mucosal antifungal host defense, our laboratory is interested in developing a better understanding of the clinical presentation, diagnostic criteria, genetics, and mechanisms of autoimmunity in CARD9 deficiency with a goal to devise mechanism-based preventative and treatment strategies for affected patients, which are tested in clinical trials at the NIH Clinical Center. Beyond CARD9 deficiency, the laboratory actively investigates the mechanisms of susceptibility to CMC in STAT1 gain-of-function mutations and DOCK8 deficiency using human and mouse studies.
With regard to invasive aspergillosis, the laboratory studies novel genetic defects that cause susceptibility to pulmonary and/or extrapulmonary infection beyond CGD and investigates the mechanisms of Aspergillus susceptibility in the setting of iatrogenic inhibition of BTK (Bruton's tyrosine kinase) in Btk-/- and Btk conditional knockout mice and in patients that are treated with the BTK inhibitors ibrutinib and acalabrutinib. Last, our lab is working with the NIAID Clinical Genomics Program with a goal to identify novel genetic variants that result in inherited susceptibility to fungal infections by Candida, Aspergillus, and other molds.
Biography
Dr. Lionakis obtained his M.D. and Sc.D. from the University of Crete in Greece. In 2002, he came to the United States and worked as a research fellow at the University of Texas MD Anderson Cancer Center (MDACC) under the mentorship of Dimitrios Kontoyiannis. At MDACC, Dr. Lionakis did clinical research on risk factors, diagnosis, and management of opportunistic fungal infections in cancer patients and bench research focusing on pharmacology and microbial factors in mouse and Drosophila models of invasive aspergillosis, fusariosis, and candidiasis.
After completing his clinical training in Internal Medicine at Baylor College of Medicine and Infectious Diseases at NIAID, Dr. Lionakis joined the Laboratory of Molecular Immunology (LMI) in 2008 and began to work on fungal immunology under the mentorship of Philip Murphy. At LMI, Dr. Lionakis did bench research on how chemotactic factors regulate the innate immune response in invasive candidiasis. In 2010, he was recruited as an Assistant Clinical Investigator in the NIAID Transition Program in Clinical Research and established the Clinical Mycology Unit within LMI. In 2012, Dr. Lionakis was recruited as a tenure-track investigator in the NIAID intramural research program and established the Fungal Pathogenesis Unit within the Laboratory of Clinical Infectious Diseases. He received tenure in 2017 and now heads the Fungal Pathogenesis Section within the Laboratory of Clinical Immunology and Microbiology.
Awards/Honors
NIAID Outstanding Mentor (2022); NIAID Merit Award (2022); National Organization for Rare Disorders (NORD) Rare Impact Award (2022); Member, Association of American Physicians (AAP) (2022); NHLBI Orloff Science Award (2022); Fellow, American Association for the Advancement of Science (AAAS) (2021); IDSA Oswald Avery Award for Early Achievement (2021); NIAID Merit Award (2020); NIH Director's Award (2020); Member, American Society for Clinical Investigation (ASCI) (2020); NIAID Merit Award (2019); Fellow, American Academy of Microbiology (AAM) (2019); NIH Director's Award (2019); NIAID Merit Award (2018); Fellow, European Confederation of Medical Mycology (FECMM) (2018); Young Investigator Award, International Immunocompromised Host Society (ICHS) (2018); American College of Physicians (ACP) Walter J. McDonald Award for Early Career Physicians (2017); Fellow of Infectious Diseases Society of America (FIDSA) (2016); IDWeek Investigator Award (2015); BeHEARD Science Prize Winner, Rare Genomics Institute (2015); 50th ICAAC George McCracken Infectious Disease Fellow Award (2010); 49th ICAAC Infectious Disease Fellows Grant Program Award (2009); Henry McIntosh Award for Outstanding Resident in Medicine (2007); Offered Chief Resident position, Baylor College of Medicine (2006); Certificate of Merit, MD Anderson Cancer Center (2004); 1st place Bristol-Myers Squibb Award in Clinical/Translational Research, Trainee Recognition Day, MD Anderson Cancer Center (2004); 43rd ICAAC Program Committee Award for Outstanding Research in the Pathogenesis of Microbial Diseases (2003); Giorgos Gennimatas Scholarship Award (2002); GlaxoWellcome Scholarship Award (2000); Lilian Voudouri Foundation Scholarship Award (2000); The Hellenic National Scholarships' Foundation Scholarship Award (2000); Dretakis Foundation Scholarship Award (2000).
Memberships
- European Confederation of Medical Mycology
- American College of Physicians
- American Society of Microbiology
- Infectious Diseases Society of America
- Mycoses Study Group
- International Immunocompromised Host Society
- International Society for Human and Animal Mycology
- American Association of Immunologists
- Clinical Immunology Society
- American Association for the Advancement of Science
Editorial Boards
- JCI Insight
- Journal of Infectious Diseases
- Infection & Immunity
- Frontiers in Cellular & Infection Microbiology
- Virulence
- Journal of Visualized Experiments
- F1000 Research (Immunology/Immunity to Infections)
- Journal of Fungi
- Antimicrobials Agents & Chemotherapy
Selected Publications
- Break TJ, Oikonomou V, Dutzan N, Desai JV, Swidergall M, Freiwald T, Chauss D, Harrison OJ, Alejo J, Williams DW, Pittaluga S, Lee CR, Bouladoux N, Swamydas M, Hoffman KW, Greenwell-Wild T, Bruno VM, Rosen LB, Lwin W, Renteria A, Pontejo SM, Shannon JP, Myles IA, Olbrich P, Ferré EMN, Schmitt M, Martin D, Genomics and Computational Biology Core, Barber DL, Solis NV, Notarangelo LD, Serreze DV, Matsumoto M, Hickman HD, Murphy PM, Anderson MS, Lim JK, Holland SM, Filler SG, Afzali B, Belkaid Y, Moutsopoulos NM, Lionakis MS. Aberrant type 1 immunity drives susceptibility to mucosal fungal infections. Science. 2021;371(6526).
- Desai JV, Kumar D, Freiwald T, Chauss D, Johnson MD, Abers MS, Steinbrink JM, Perfect JR, Alexander B, Matzaraki V, Snarr BD, Zarakas MA, Oikonomou V, Silva LM, Shivarathri R, Beltran E, Demontel LN, Wang L, Lim JK, Launder D, Conti HR, Swamydas M, McClain MT, Moutsopoulos NM, Kazemian M, Netea MG, Kumar V, Köhl J, Kemper C, Afzali B, Lionakis MS. C5a-licensed phagocytes drive sterilizing immunity during systemic fungal infection. Cell. 2023;186(13):2802-2822.e22.
- Oikonomou V, Smith G, Constantine GM, Schmitt MM, Ferré EMN, Alejo JC, Riley D, Kumar D, Dos Santos Dias L, Pechacek J, Hadjiyannis Y, Webb T, Seifert BA, Ghosh R, Walkiewicz M, Martin D, Besnard M, Snarr BD, Deljookorani S, Lee CR, DiMaggio T, Barber P, Rosen LB, Cheng A, Rastegar A, de Jesus AA, Stoddard J, Kuehn HS, Break TJ, Kong HH, Castelo-Soccio L, Colton B, Warner BM, Kleiner DE, Quezado MM, Davis JL, Fennelly KP, Olivier KN, Rosenzweig SD, Suffredini AF, Anderson MS, Swidergall M, Guillonneau C, Notarangelo LD, Goldbach-Mansky R, Neth O, Monserrat-Garcia MT, Valverde-Fernandez J, Lucena JM, Gomez-Gila AL, Garcia Rojas A, Seppänen MRJ, Lohi J, Hero M, Laakso S, Klemetti P, Lundberg V, Ekwall O, Olbrich P, Winer KK, Afzali B, Moutsopoulos NM, Holland SM, Heller T, Pittaluga S, Lionakis MS. The Role of Interferon-γ in Autoimmune Polyendocrine Syndrome Type 1. N Engl J Med. 2024;390(20):1873-1884.
- Drummond RA, Swamydas M, Oikonomou V, Zhai B, Dambuza IM, Schaefer BC, Bohrer AC, Mayer-Barber KD, Lira SA, Iwakura Y, Filler SG, Brown GD, Hube B, Naglik JR, Hohl TM, Lionakis MS. CARD9(+) microglia promote antifungal immunity via IL-1β- and CXCL1-mediated neutrophil recruitment. Nat Immunol. 2019;20(5):559-570.
- Desai JV, Zarakas MA, Wishart AL, Roschewski M, Aufiero MA, Donkò A, Wigerblad G, Shlezinger N, Plate M, James MR, Lim JK, Uzel G, Bergerson JR, Fuss I, Cramer RA, Franco LM, Clark ES, Khan WN, Yamanaka D, Chamilos G, El-Benna J, Kaplan MJ, Staudt LM, Leto TL, Holland SM, Wilson WH, Hohl TM, Lionakis MS. BTK drives neutrophil activation for sterilizing antifungal immunity. J Clin Invest. 2024;134(12).
Related Scientific Focus Areas

Microbiology and Infectious Diseases
View additional Principal Investigators in Microbiology and Infectious Diseases


This page was last updated on Friday, July 25, 2025