
Research Topics
The major focus of the HIV-Specific Immunity Section is identifying the mechanisms of an effective humoral and cellular immune response to HIV. Identifying the components, targets, and magnitude of such responses is a critical step toward the development of effective vaccines and immunotherapies. In our investigation, we recruit patients who are the best available examples of effective humoral or cellular responses to HIV and study their immune response in detail. The knowledge provided by this work offers fundamental insights about the regulation of human immune responses to HIV and other viruses.
Mechanisms of Immunologic Restriction of HIV replication
(Stephen A. Migueles, M.D., Lead Investigator)
A number of recent studies have provided evidence for the role of CD8+ T cells in restricting lentivirus replication in vivo; however, the reason the CD8+ T-cell response fails to control HIV in the majority of infected individuals remains incompletely understood. It is now clear that there exists a group of rare patients who maintain immunologic restriction of HIV replication, despite prolonged infection, without the use of antiretroviral therapy. Many of these patients have been infected for more than 20 years with no CD4+ T-cell decline. These patients, referred to as long-term nonprogressors (LTNP), or “elite controllers,” likely hold important clues to the components of an effective immune response to HIV.
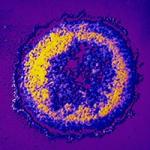
Credit: NIAIDNIAID is recruiting volunteers for a study that will examine how the immune system controls HIV infection.Conversely, they also hold important clues regarding how control of HIV replication is lost in most infected individuals. We have now assembled a large cohort of patients with nonprogressive infection. Cells from these patients, as well as from major histocompatibility complex (MHC) matched and mismatched progressors as controls, are being used to systematically dissect the mechanisms of immune-mediated restriction of HIV replication.
Major Findings
- Within our cohort of LTNP is a dramatic overrepresentation of the B*5701 class I allele: 68 percent compared to 11 percent in the caucasian U.S. population.
- CD8+ T-cell response to HIV-1 in LTNP is more narrow (typically directed toward three to four epitopes) than the response in progressors (typically 15 to 20 epitopes).
- CD8+ T-cell response of LTNP is highly focused on peptides restricted by the B*5701 allele, in most cases to the exclusion of peptides restricted by other alleles.
- Very high frequencies of circulating CD8+ T cells (0.8 to 18 percent IFN-g producing) were found to be HIV-specific in both LTNP and progressors, suggesting the difference in effectiveness of patients’ responses is qualitative rather than quantitative.
- The autologous virus is recognized by a high-frequency response in both patient groups. There are no differences between patient groups in the frequency of putative “escape mutations.”
- LTNP are distinguished by the maintenance of HIV-specific CD8+ T cells with a high proliferative capacity. This proliferation was found to be coupled to or parallel to perforin expression.
- HIV-specific CD4+ T cells in treated progressors are similar in frequency, function, and phenotype to those in LTNP and to non-HIV specific responses in uninfected controls.
- LTNP/EC are distinguished from progressors by a dramatic difference in CD8+ T-cell-mediated killing of HIV-infected cells. This difference in killing is mediated by the granule-exocytosis pathway through differences in perforin and granzyme B production.
- Cytotoxic killing of HIV-infected cells is a leading candidate for an immune correlate of vaccine-induced immunologic control of HIV.
Mechanisms of broad cross-neutralization of HIV
(Jinghe Huang, Ph.D., Lead Investigator)
There is a growing consensus that eliciting both neutralizing antibodies (NtAb) and a potent T-cell response will be necessary for an effective HIV vaccine. Eliciting NtAb to HIV, however, has been a challenging goal. Thus far, efforts to determine the mechanism(s) of broad cross-neutralization by patient sera have been hampered by a number of obstacles, including a lack of cohorts with broad responses, a lack of techniques to purify antigen-specific cells, and inefficient cloning techniques. Our work has overcome a number of these obstacles and is permitting a careful study of specificities that mediate broad cross-neutralization. Determining the specificities of these antibodies will likely be critical for the design of effective HIV vaccines.
Major Findings
- Broad cross-neutralizaiton of HIV is not rare and can be found in up to 20 percent of HIV-infected patients.
- Antibody-dependent cellular cytotoxicity against primary HIV-infected cells is directly associated with the magnitude of surface IgG binding.
- Cloning of individual memory B cells from patients with broadly cross-neutralizing antibodies is resulting in isolation of antibodies capable of neutralizing 98 percent of tested strains.
- Broad and potent monoclonal antibodies are providing important clues regarding the best targets within the HIV envelope protein to mediate a broad neutralization of HIV. The specificities of these antibodies have very important implications for the design of vaccines against HIV-1.
Biography
Dr. Connors received his M.D. from Temple University and was trained in pediatrics at Tufts New England Medical Center. He joined the NIAID Laboratory of Infectious Diseases in 1989 to study the immune response to respiratory syncytial virus. He was trained in infectious diseases at the National Institutes of Health Clinical Center and at the Children’s Hospital of Philadelphia. He joined the Laboratory of Immunoregulation in 1994 to study the human immune response to HIV. Dr. Connors has published a series of discoveries that have laid the framework for current understanding of immunologic control of HIV in some rare patients and loss of immunologic control in the majority of infected patients.
Selected Publications
- Migueles SA, Nettere DM, Gavil NV, Wang LT, Toulmin SA, Kelly EP, Ward AJ, Lin S, Thompson SA, Peterson BA, Abdeen CS, Sclafani CR, Pryal PF, Leach BG, Ludwig AK, Rogan DC, Przygonska PA, Cattani A, Imamichi H, Sachs A, Cafri G, Huang NN, Patamawenu A, Liang CJ, Hallahan CW, Kambach DM, Han EX, Coupet T, Chen J, Moir SL, Chun TW, Coates EE, Ledgerwood J, Schmidt J, Taillandier-Coindard M, Michaux J, Pak H, Bassani-Sternberg M, Frahm N, McElrath MJ, Connors M. HIV vaccines induce CD8(+) T cells with low antigen receptor sensitivity. Science. 2023;382(6676):1270-1276.
- Huang J, Kang BH, Ishida E, Zhou T, Griesman T, Sheng Z, Wu F, Doria-Rose NA, Zhang B, McKee K, O'Dell S, Chuang GY, Druz A, Georgiev IS, Schramm CA, Zheng A, Joyce MG, Asokan M, Ransier A, Darko S, Migueles SA, Bailer RT, Louder MK, Alam SM, Parks R, Kelsoe G, Von Holle T, Haynes BF, Douek DC, Hirsch V, Seaman MS, Shapiro L, Mascola JR, Kwong PD, Connors M. Identification of a CD4-Binding-Site Antibody to HIV that Evolved Near-Pan Neutralization Breadth. Immunity. 2016;45(5):1108-1121.
- Huang J, Ofek G, Laub L, Louder MK, Doria-Rose NA, Longo NS, Imamichi H, Bailer RT, Chakrabarti B, Sharma SK, Alam SM, Wang T, Yang Y, Zhang B, Migueles SA, Wyatt R, Haynes BF, Kwong PD, Mascola JR, Connors M. Broad and potent neutralization of HIV-1 by a gp41-specific human antibody. Nature. 2012;491(7424):406-12.
- Migueles SA, Osborne CM, Royce C, Compton AA, Joshi RP, Weeks KA, Rood JE, Berkley AM, Sacha JB, Cogliano-Shutta NA, Lloyd M, Roby G, Kwan R, McLaughlin M, Stallings S, Rehm C, O'Shea MA, Mican J, Packard BZ, Komoriya A, Palmer S, Wiegand AP, Maldarelli F, Coffin JM, Mellors JW, Hallahan CW, Follman DA, Connors M. Lytic granule loading of CD8+ T cells is required for HIV-infected cell elimination associated with immune control. Immunity. 2008;29(6):1009-21.
- Matsuda K, Migueles SA, Huang J, Bolkhovitinov L, Stuccio S, Griesman T, Pullano AA, Kang BH, Ishida E, Zimmerman M, Kashyap N, Martins KM, Stadlbauer D, Pederson J, Patamawenu A, Wright N, Shofner T, Evans S, Liang CJ, Candia J, Biancotto A, Fantoni G, Poole A, Smith J, Alexander J, Gurwith M, Krammer F, Connors M. A replication-competent adenovirus-vectored influenza vaccine induces durable systemic and mucosal immunity. J Clin Invest. 2021;131(5).
Related Scientific Focus Areas

Microbiology and Infectious Diseases
View additional Principal Investigators in Microbiology and Infectious Diseases


This page was last updated on Thursday, September 19, 2024