
Research Topics
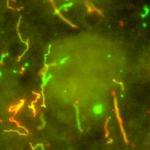
Virus infection of the Central Nervous System (CNS) can lead to damage to neurons and the development of neurological disease. Multiple cell types in the CNS are activated during virus infection and have important roles in regulating viral pathogenesis. The goal of our laboratory is to examine the interactions between the immune and nervous systems in regulating viral pathogenesis with the ultimate goal of identifying targets for therapeutic treatment of viral-mediated neurological diseases. We primarily utilize two different models of viral infections that mediate neuronal damage via either direct or indirect mechanisms. One model utilizes La Crosse Virus (LACV), a bunyavirus that is one of the leading causes of pediatric viral encephalitis in the United States. LACV induces neuronal apoptosis by directly infecting neurons. The other model of viral neuropathogenesis is a retrovirus model, where microglia and macrophages are the primary cell type infected in the CNS. In this model system, the damage to neurons is indirect. Our work with these viruses has identified mechanisms of both neuronal damage and neuronal protection that are mediated by specific interactions of the immune system with cells of the central nervous system. We are currently examining the regulation of these pathways and mechanisms in order to inhibit viral pathogenesis in the CNS.
Biography
Karin Peterson received her Ph.D. degree in microbiology and immunology in 1998 from the University of Missouri Medical School, where she studied autoimmunity and the activation of self-reactive T cells. She then went to Rocky Mountain Laboratories (RML) in 1998 as a postdoctoral fellow in the Laboratory of Persistent Viral Diseases and applied her skills in immunology toward understanding the mechanisms that control the immune response to retrovirus infection. During this time, she became interested in the immune responses to virus infections in the central nervous system (CNS). In 2004, Dr. Peterson accepted a position as an assistant professor at Louisiana State University School of Veterinary Medicine, where she furthered her studies on viral pathogenesis in the CNS and also taught classes in immunology and virology. In 2008, she returned to RML as a tenure-track investigator to study the innate immune responses in the CNS and their role in viral pathogenesis.
Selected Publications
- Ojha D, Winkler CW, Leung JM, Woods TA, Chen CZ, Nair V, Taylor K, Yeh CD, Tawa GJ, Larson CL, Zheng W, Haigh CL, Peterson KE. Rottlerin inhibits La Crosse virus-induced encephalitis in mice and blocks release of replicating virus from the Golgi body in neurons. Nat Microbiol. 2021;6(11):1398-1409.
- Schneider CA, Leung JM, Valenzuela-Leon PC, Golviznina NA, Toso EA, Bosnakovski D, Kyba M, Calvo E, Peterson KE. Skin muscle is the initial site of viral replication for arboviral bunyavirus infection. Nat Commun. 2024;15(1):1121.
- Ojha D, Hill CS, Zhou S, Evans A, Leung JM, Schneider CA, Amblard F, Woods TA, Schinazi RF, Baric RS, Peterson KE, Swanstrom R. N4-Hydroxycytidine/molnupiravir inhibits RNA virus-induced encephalitis by producing less fit mutated viruses. PLoS Pathog. 2024;20(9):e1012574.
- Mukherjee P, Woods TA, Moore RA, Peterson KE. Activation of the innate signaling molecule MAVS by bunyavirus infection upregulates the adaptor protein SARM1, leading to neuronal death. Immunity. 2013;38(4):705-16.
- Winkler CW, Woods TA, Groveman BR, Carmody AB, Speranza EE, Martens CA, Best SM, Haigh CL, Peterson KE. Neuronal maturation reduces the type I IFN response to orthobunyavirus infection and leads to increased apoptosis of human neurons. J Neuroinflammation. 2019;16(1):229.
Related Scientific Focus Areas
Microbiology and Infectious Diseases
View additional Principal Investigators in Microbiology and Infectious Diseases




Molecular Biology and Biochemistry
View additional Principal Investigators in Molecular Biology and Biochemistry
This page was last updated on Wednesday, August 13, 2025