
Ian A. Myles, M.D., M.P.H.
Lasker Clinical Research Scholar
Epithelial Therapeutics Unit
NIAID/DIR
Research Topics
Our group focuses on how human health is affected by the normal microorganisms that live on our skin (collectively termed the microbiome). Our emphasis is on eczema (also called atopic dermatitis or AD), which is an inflammatory disease of the skin associated with reduced quality of life and high risk of developing asthma, allergic rhinitis, and food allergies. AD afflicts 5 to 25 percent of children globally and has a reported prevalence of 8 to 18 percent in the United States. Patients with AD require increased health care utilization, suffering substantially greater out-of-pocket costs than matched controls. The underlying pathology of AD includes defective skin barrier function, susceptibility to Staphylococcus aureus skin infection, and immune dysregulation. Current therapeutic options are limited by their requirement for multiple-times-per-day applications and/or substantial cost. While the natural history of AD suggests that 50 to 90 percent of patents will self-resolve by approximately 10 to 15 years of age, the prolonged barrier defects may put patients at risk for development of associated allergic diseases.
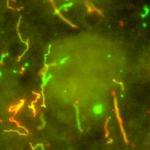
Recent work has uncovered that the skin microbiome is significantly different between healthy controls and patients with AD and that early commensal diversity may protect against development of AD. These realizations suggest that the skin microbiome contributes to AD presentation through both harmful and protective pathways. Our group identified a species of bacteria from normal healthy skin, called Roseomonas mucosa, which showed promising features in cell culture and mouse models that suggested the bacteria might be able to treat patients with eczema. We have since transitioned into a clinical trial using Roseomonas mucosa as a topical treatment for eczema. While guided by the science, our group strives to find treatments that not only improve symptoms but also provide relief without worsening the financial and/or time burdens that disease places on patients and their families.
Beyond the immediate clinical trial, our group is interested in the role the microbiome plays in normal tissue repair and wound healing. The skin, the colon, and the lungs all have to 'renew' themselves naturally due to normal day-to-day wear-and-tear. These tissues cannot correctly do so without contact with various microorganisms, and we endeavor to better understand why. Furthermore, we are interested in how environmental factors can influence health through effects on the microbiome. For example, we are interested in uncovering how a healthy diet encourages the types of microorganisms that support good health. This includes not only dietary fats and sugars, but also early exposures like breast milk. We also work to uncover what chemical exposures (such as soaps or topical preservatives) may benefit or harm the microbial balance in ways that influence health and disease.
Biography
Dr. Myles was born and raised in Colorado. He graduated with a B.S. in biology from Colorado State University in 2001 and then obtained an M.D. from the University of Colorado in 2005. He completed an internal medicine residency at The Ohio State University prior to beginning fellowship training in allergy and clinical immunology at NIH. He worked under the mentorship of Dr. Sandip Datta investigating the mechanistic details of susceptibility to S. aureus skin infections. In 2011, Dr. Myles became a commissioned officer in the United States Public Health Service Commissioned Corps. LCDR Myles has supported several USPHS missions, from the Ebola virus vaccine trial in West Africa to congressional Gold Medal Ceremonies at the U.S. Capitol. In 2013, he was awarded a position as an assistant clinical investigator in the NIAID Transition Program in Clinical Research. Dr. Myles received his M.P.H. from George Washington University in 2016. In 2018, Dr. Myles became the head of the newly formed Epithelial Therapeutics Unit to evaluate the efficacy and safety of a topical, live bacterial treatment for atopic dermatitis (eczema). He is currently a participant in the Lasker Clinical Research Scholars and Distinguished Scholars programs.
Selected Publications
- Zeldin J, Chaudhary PP, Spathies J, Yadav M, D'Souza BN, Alishahedani ME, Gough P, Matriz J, Ghio AJ, Li Y, Sun AA, Eichenfield LF, Simpson EL, Myles IA. Exposure to isocyanates predicts atopic dermatitis prevalence and disrupts therapeutic pathways in commensal bacteria. Sci Adv. 2023;9(1):eade8898.
- Myles IA, Earland NJ, Anderson ED, Moore IN, Kieh MD, Williams KW, Saleem A, Fontecilla NM, Welch PA, Darnell DA, Barnhart LA, Sun AA, Uzel G, Datta SK. First-in-human topical microbiome transplantation with Roseomonas mucosa for atopic dermatitis. JCI Insight. 2018;3(9).
- Myles IA, Castillo CR, Barbian KD, Kanakabandi K, Virtaneva K, Fitzmeyer E, Paneru M, Otaizo-Carrasquero F, Myers TG, Markowitz TE, Moore IN, Liu X, Ferrer M, Sakamachi Y, Garantziotis S, Swamydas M, Lionakis MS, Anderson ED, Earland NJ, Ganesan S, Sun AA, Bergerson JRE, Silverman RA, Petersen M, Martens CA, Datta SK. Therapeutic responses to Roseomonas mucosa in atopic dermatitis may involve lipid-mediated TNF-related epithelial repair. Sci Transl Med. 2020;12(560).
- Myles IA, Anderson ED, Earland NJ, Zarember KA, Sastalla I, Williams KW, Gough P, Moore IN, Ganesan S, Fowler CJ, Laurence A, Garofalo M, Kuhns DB, Kieh MD, Saleem A, Welch PA, Darnell DA, Gallin JI, Freeman AF, Holland SM, Datta SK. TNF overproduction impairs epithelial staphylococcal response in hyper IgE syndrome. J Clin Invest. 2018;128(8):3595-3604.
- Myles IA, Datta SK. Frontline Science: Breast milk confers passive cellular immunity via CD8-dependent mechanisms. J Leukoc Biol. 2021;109(4):709-715.
Related Scientific Focus Areas

Microbiology and Infectious Diseases
View additional Principal Investigators in Microbiology and Infectious Diseases
This page was last updated on Wednesday, January 31, 2024