Gregory George Germino, M.D.
Senior Investigator
Kidney Diseases Branch
NIDDK
Institute Deputy Director
NIDDK
Research Topics
Current Research
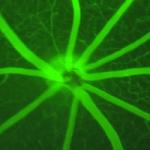
The function of the kidney critically depends on the proper structure of its tubule system, yet regulation of tubular diameter is a poorly understood phenomenon. Cystic diseases of the kidney offer unique opportunities to study these processes. My research focuses on the molecular basis of renal cystic disease and renal tubular morphogenesis.
Autosomal dominant polycystic kidney disease (ADPKD) affects approximately 1/1000 Americans. Cysts arise at all stages of life, and gradually expand to replace normal renal parenchyma. This process results in end stage kidney failure (ESKF) in approximately half by the 6th decade, accounting for approximately 5 percent of all cases of ESKF. Autosomal recessive polycystic kidney disease (ARPKD) is rare (1/20,000) but often more severe. Therapies for both are limited to managing the complications. We have, however, made great progress in understanding their pathobiology and the role of the normal PKD gene products in regulating tubular morphology.
Mutations in either of two genes, PKD1 and PKD2, cause most forms of ADPKD. Mutations appear to compromise gene function, and much data implicate a molecular recessive model as responsible for initiating cyst growth. PKD1 and PKD2 encode components of a receptor-channel complex that likely has ciliary and non-ciliary functions. Using orthologous mouse models, we have demonstrated unsuspected, complex development-stage specific consequences of Pkd1 inactivation that are linked to metabolic pathways. These models also have been used to show that PKD genes are essential for proper form and function of multiple other organs. We are pursuing several parallel lines of inquiry regarding the relationship between PKD proteins, cellular metabolism, matrix, and planar cell polarity pathways.
ARPKD is a second interest. We identified the gene mutated in this disorder, PKHD1, and have shown that it likely encodes a very large membrane-associated protein that undergoes Notch-like proteolytic processing. We have developed a series of mouse lines and cell culture systems to model the disease and study the protein, and we have shown genetic interaction between the PKD1 and PKHD1 loci. Current efforts are focused on determining its function in kidney and liver development.
Biography
- Senior Investigator, Kidney Diseases Branch, NIDDK, NIH, 2009–Present
- Adjunct Professor of Medicine, Johns Hopkins University School of Medicine, 2009–Present
- Professor of Medicine, Division of Nephrology, Johns Hopkins University School of Medicine, 2003–2009
- Affiliate Member, McKusick-Nathans Institute of Genetic Medicine, Johns Hopkins University School of Medicine, 2002–2009
- Joint Appointment, Department of Molecular Biology and Genetics, Johns Hopkins University School of Medicine, 2001–2009
- Associate Professor of Medicine, Division of Nephrology, Johns Hopkins University School of Medicine, 1997–2003
- Assistant Professor of Medicine, Division of Nephrology, Johns Hopkins University School of Medicine, 1992–1997
- Associate Research Scientist, Instructor and Assistant Professor, Yale University School of Medicine, 1988–1992
- Research Post-Doctoral Fellow, Nuffield Department of Medicine, Oxford University, 1987–1988
- Clinical Post-Doctoral Fellow, Nephrology, Yale University School of Medicine, 1986–1987
- Internal Medicine Residency, Yale–New Haven Hospital, 1983–1986
- M.D., University of Chicago Pritzker School of Medicine, 1983
- B.S., Loyola University of Chicago, 1979
Selected Publications
- Menezes LF, Germino GG. The pathobiology of polycystic kidney disease from a metabolic viewpoint. Nat Rev Nephrol. 2019;15(12):735-749.
- Lin CC, Kurashige M, Liu Y, Terabayashi T, Ishimoto Y, Wang T, Choudhary V, Hobbs R, Liu LK, Lee PH, Outeda P, Zhou F, Restifo NP, Watnick T, Kawano H, Horie S, Prinz W, Xu H, Menezes LF, Germino GG. A cleavage product of Polycystin-1 is a mitochondrial matrix protein that affects mitochondria morphology and function when heterologously expressed. Sci Rep. 2018;8(1):2743.
- Menezes LF, Lin CC, Zhou F, Germino GG. Fatty Acid Oxidation is Impaired in An Orthologous Mouse Model of Autosomal Dominant Polycystic Kidney Disease. EBioMedicine. 2016;5:183-92.
- Ishimoto Y, Menezes LF, Zhou F, Yoshida T, Komori T, Qiu J, Young MF, Lu H, Potapova S, Outeda P, Watnick T, Germino GG. A novel ARPKD mouse model with near-complete deletion of the Polycystic Kidney and Hepatic Disease 1 (Pkhd1) genomic locus presents with multiple phenotypes but not renal cysts. Kidney Int. 2023.
- Menezes LF, Zhou F, Patterson AD, Piontek KB, Krausz KW, Gonzalez FJ, Germino GG. Network analysis of a Pkd1-mouse model of autosomal dominant polycystic kidney disease identifies HNF4α as a disease modifier. PLoS Genet. 2012;8(11):e1003053.
Related Scientific Focus Areas



Molecular Biology and Biochemistry
View additional Principal Investigators in Molecular Biology and Biochemistry
This page was last updated on Thursday, August 7, 2025