Research Topics
Dr. Mezey is interested in the biology of bone marrow stromal cells (MSCs). These cells are able to suppress the immune system and have been tested in autoimmune diseases. The same cells also support hematopoiesis (making of blood cells) in the bone marrow. Her studies suggest that injected MSCs might be able to alleviate sepsis in patients. Studies also reveal that—through a different mechanism—these cells might reduce the symptoms of asthma. Her group studies ways in which to improve the efficiency of these cells in fighting auto-immune diseases. In addition, they are studying how MSCs might regulate red cell production in the bone marrow of patients with anemia. Dr. Mezey’s group collaborates with clinicians to find out the best ways to use the unique properties of these cells in patients, and to prime MSCs for targeted use.
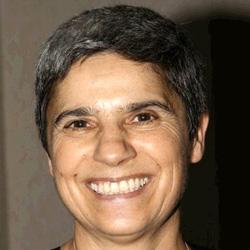
Biography
Dr. Éva Mezey earned her M.D. from the Semmelweis University Medical School in Budapest, Hungary, where she taught neuroanatomy, and began doing research under the guidance of Drs. Janos Szentagothai and Miklos Palkovits. She then worked with Prof. David DeWied in Utrecht. Dr. Mezey received a Ph.D. in neuroendocrinology from the Hungarian Academy of Sciences. Dr. Mezey came to NIH as a postdoctoral fellow in the Laboratory of Cell Biology at NIMH and later at NINDS. At NIDCR, Dr. Mezey established the Adult Stem Cell Section to study the biology of bone marrow derived stem cells (MSCs). Dr. Mezey has received a Doctor of Science (D.Sc.) degree and has been elected to the Hungarian Academy of Sciences. She is a member of the International Stem Cell Society and the Society for Neuroscience.
Selected Publications
- Mezey E, Chandross KJ, Harta G, Maki RA, McKercher SR. Turning blood into brain: cells bearing neuronal antigens generated in vivo from bone marrow. Science. 2000;290(5497):1779-82.
- Németh K, Leelahavanichkul A, Yuen PS, Mayer B, Parmelee A, Doi K, Robey PG, Leelahavanichkul K, Koller BH, Brown JM, Hu X, Jelinek I, Star RA, Mezey E. Bone marrow stromal cells attenuate sepsis via prostaglandin E(2)-dependent reprogramming of host macrophages to increase their interleukin-10 production. Nat Med. 2009;15(1):42-9.
- Mayer B, Németh K, Krepuska M, Myneni VD, Maric D, Tisdale JF, Hsieh MM, Uchida N, Lee HJ, Nemeth MJ, Holmbeck K, Noguchi CT, Rogers H, Dey S, Hansen A, Hong J, Chow I, Key S, Szalayova I, Pagani J, Markó K, McClain-Caldwell I, Vitale-Cross L, Young WS, Brownstein MJ, Mezey É. Vasopressin stimulates the proliferation and differentiation of red blood cell precursors and improves recovery from anemia. Sci Transl Med. 2017;9(418).
- Mezey É, Szalayova I, Hogden CT, Brady A, Dósa Á, Sótonyi P, Palkovits M. An immunohistochemical study of lymphatic elements in the human brain. Proc Natl Acad Sci U S A. 2021;118(3).
- Vitale-Cross L, Szalayova I, Scoggins A, Palkovits M, Mezey E. SARS-CoV-2 entry sites are present in all structural elements of the human glossopharyngeal and vagal nerves: Clinical implications. EBioMedicine. 2022;78:103981.
Related Scientific Focus Areas


Microbiology and Infectious Diseases
View additional Principal Investigators in Microbiology and Infectious Diseases
This page was last updated on Wednesday, March 26, 2025