Research Topics
Within the scope of his glioma research at the Neuro-Oncology Branch (NOB), Dr. Yang has designed a multifaceted approach to not only understand disease biology, but also steer laboratory research in a translationally-relevant direction.
The first primary focus within Dr. Yang’s lab involves using DNA repair inhibitors to sensitize glioma cells to radiation and chemotherapy. The goal of this work is to use multi-omic techniques with patient derived cell lines, tissue specimens, and bioinformatics to shed light on the transcriptomic, metabolic, and biochemical differences between glioma subtypes.
Additionally, Dr. Yang has been focused on the neomorphic activity (that is, the change in function) of the IDH enzyme, as well as its oncometabolite 2-hydroxyglutarate (2-HG) and its role in cancer biology and therapeutic vulnerabilities. Dr. Yang’s recent findings suggest that administering an FDA-approved PARP inhibitor (a DNA repair inhibitor) could result in synthetic lethality in IDH-mutant glioma cells, which improves therapeutic response with reduced tumor expansion.
Another broad research endeavor in Dr. Yang’s laboratory is identifying the metabolic and biological vulnerabilities of IDH-mutant glioma cells, in order to understand how these cells develop a protective shield and avoid being maximally impacted by therapy. Research has shown that NRF2, a transcription factor, could be a critical driver for survival in IDH-mutant tumors, and Dr. Yang’s findings suggest that targeting NRF2 results in more profound cytotoxicity in preclinical mouse models. Dr. Yang is also collaborating with other research groups within the NCI Center for Cancer Research’s Neuro-Oncology Branch (NOB) and the NCI more broadly to develop reliable IDH-mutant glioma mouse models that will be essential for studying the disease and potential treatments in a preclinical setting.
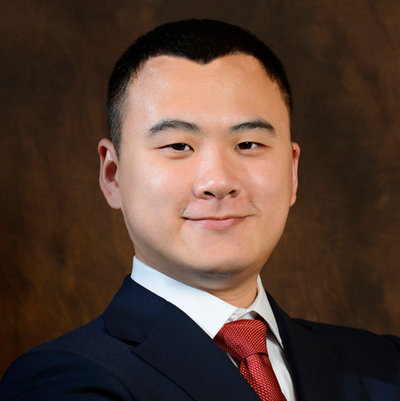
Biography
Dr. Yang obtained his Ph.D. in neurobiology from Peking University in China immediately after earning a Bachelor of Science in medicine at the same institution. Motivated by a family member’s brain tumor diagnosis, he moved to the NIH shortly after completing his degrees to pursue a postdoctoral fellowship at the Surgical Neurology Branch under National Institutes of Neurological Disorders and Stroke. During this time, Dr. Yang led several research projects to understand the biology of neurological diseases and central nervous system tumors, in hopes of developing a therapeutic regimen optimized for these diseases. Following his postdoctoral fellowship in 2016, he joined the Neuro-Oncology Branch (NOB) as an investigator, and has led the Molecular and Cell Biology Program ever since.
In addition to his research, Dr. Yang is also part of several societies, such as the American Association for Cancer Research and the Society for Neuro-Oncology. He has received several awards during his time at the NIH, including a Distinguished Scientist Award and a Young Investigator Award for his postdoctoral research.
Select Societies and Initiatives
- NIH DNA Repair Interest Group
- American Association for Cancer Research (AACR)
- Society for Neuro-Oncology (SNO)
- Society of Chinese Bioscientists in America (SCBA)
Selected Publications
- Yang C, Huntoon K, Ksendzovsky A, Zhuang Z, Lonser RR. Proteostasis modulators prolong missense VHL protein activity and halt tumor progression. Cell Rep. 2013;3(1):52-9.
- Yang C, Rahimpour S, Lu J, Pacak K, Ikejiri B, Brady RO, Zhuang Z. Histone deacetylase inhibitors increase glucocerebrosidase activity in Gaucher disease by modulation of molecular chaperones. Proc Natl Acad Sci U S A. 2013;110(3):966-71.
- Yang C, Asthagiri AR, Iyer RR, Lu J, Xu DS, Ksendzovsky A, Brady RO, Zhuang Z, Lonser RR. Missense mutations in the NF2 gene result in the quantitative loss of merlin protein and minimally affect protein intrinsic function. Proc Natl Acad Sci U S A. 2011;108(12):4980-5.
- Yang C, Iyer RR, Yu AC, Yong RL, Park DM, Weil RJ, Ikejiri B, Brady RO, Lonser RR, Zhuang Z. β-Catenin signaling initiates the activation of astrocytes and its dysregulation contributes to the pathogenesis of astrocytomas. Proc Natl Acad Sci U S A. 2012;109(18):6963-8.
- Zhuang Z, Yang C, Lorenzo F, Merino M, Fojo T, Kebebew E, Popovic V, Stratakis CA, Prchal JT, Pacak K. Somatic HIF2A gain-of-function mutations in paraganglioma with polycythemia. N Engl J Med. 2012;367(10):922-30.
Related Scientific Focus Areas




Molecular Biology and Biochemistry
View additional Principal Investigators in Molecular Biology and Biochemistry
This page was last updated on Tuesday, August 5, 2025