Research Topics
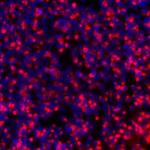
The Section on Developmental Genetics conducts laboratory and clinical investigations into a group of the most common neurodegenerative lysosomal storage disorders (LSDs), which mostly affect children. Our research currently focuses on understanding the molecular mechanisms of pathogenesis of Neuronal Ceroid Lipofuscinoses (NCLs), commonly known as Batten disease. Mutations in >13 different genes (called the CLNs) underlie various types of NCLs. Currently, there is no effective treatment for any of the NCLs. Interestingly, all NCL types share some common pathologic features. For example, intracellular accumulation of autofluorescent material, epileptic seizures, progressive psychomotor decline, visual impairment due to retinal degeneration and premature death. We first started investigating the infantile NCL (or INCL), which is caused by mutations in the CLN1 gene encoding a lysosomal depalmitoylating enzyme, palmitoyl-protein thioesterase-1 (PPT1). PPT1 catalyzes the cleavage of thioester linkage, which attaches long-chain fatty acids (predominantly palmitate) to specific cysteine residues in proteins that require palmitoylation (S-acylation) for their function. However, palmitoylated proteins are refractory to degradation by lysosomal hydrolases and PPT1-deficiency leads to lysosomal accumulation of these lipidated proteins (constituents of ceroid) leading to INCL pathogenesis. Children afflicted with INCL are normal at birth but, by 11 to 18 months of age, they exhibit signs of psychomotor retardation. By 2 years of age, they are completely blind due to retinal degeneration and, by age 4, they manifest no brain activity and remain in a vegetative state for 6 to 8 more years before eventual death. These grim outcomes underscore the urgent need for the development of rational and effective therapeutic strategies not only for INCL but also for all NCLs.
The aim of our clinical studies is to apply the knowledge gained from laboratory investigations to develop novel therapeutic strategies for Batten disease. The results of our earlier investigations led to a bench-to-bedside clinical trial, which is recently completed and the results published in Lancet Neurology. Using Cln1-knockout (Cln1-/-) mice, which recapitulate virtually all clinical and pathological features of INCL, we discovered that PPT1 deficiency causes endoplasmic reticulum (ER) and oxidative stress, which at least in part causes neuronal death by apoptosis. We also delineated a mechanism by which PPT1 deficiency disrupts the recycling of the synaptic vesicle (SV) proteins, which are essential for regenerating fresh SVs to replenish the SV pool size at the nerve terminals to maintain uninterrupted neurotransmission. We also discovered that ER and oxidative stresses contribute to neuronal apoptosis and neuroinflammation in INCL. Further, we uncovered that Ppt1 deficiency causes misrouting of the V0a1 subunit of v-ATPase (the proton pump on lysosomal membrane), which regulates lysosomal acidic pH, causing elevated pH that adversely affect lysosomal degradative function. We also discovered that nucleophilic small molecules with antioxidant properties ameliorate the neurological abnormalities in Cln1-/- mice and extend their lifespan. These and other related studies provide insight into the complex mechanisms of heritable disorders of neurodegeneration like INCL and identify several potential therapeutic targets. Our ongoing laboratory and clinical investigations are attempting to advance our knowledge of CLN1-, CLN3- and CLN10-diseases. We plan to apply new findings from our laboratory studies to develop novel therapeutic strategies not only for INCL but also for other related diseases.
Biography
Anil B. Mukherjee, M.D., Ph.D., is a Senior Investigator and Head of the Section on Developmental Genetics, NICHD. This Section conducts both laboratory and clinical investigations. The basic research is conducted to understand the molecular mechanism(s) of heritable neurodegenerative lysosomal storage disorders that mostly affect children. Current research focuses primarily on infantile neuronal ceroid lipofuscinosis (INCL) and juvenile NCL (JNCL), both devastating neurodegenerative storage diseases caused by mutations in the CLN1 and CLN3 genes, respectively, cause INCL and JNCL. The CLN1 gene encodes palmitoyl-protein thioesterase-1 (PPT1) and the CLN3 gene encodes a protein of 438 amino acids also called batenin. The biological function of this protein remains unclear. The laboratory research of Dr. Mukherjee and his colleagues uncovered that PPT1-deficiency leads endoplasmic reticulum and oxidative stress, which triggers unfolded protein response mediating neuronal death by apoptosis. A few years ago, researchers in this section screened many small molecules that functionally mimic PPT1. Based on results of their laboratory investigations, the Section was awarded the first NICHD “bench-to-bedside award” to conduct a clinical trial to determine if a combined regimen of Cystagon™ (cysteamine bitartrate) and Mucomyst® (N-acetylcysteine) is beneficial for patients with INCL. This study has recently been completed and the results published in Lancet Neurology. More recently, efforts to identify and characterize non-toxic small molecules, which mimic PPT1 activity, led to the discovery of N-tert (Butyl) hydroxylamine (NtBuHA), which protects neurons and extend the lifespan of Cln1-/- mice, a reliable animal model of INCL. Since many INCL patients in the US carry non-sense mutations in the CLN1 gene and increasingly, nonsense-suppressing small molecules are being developed, Mukherjee lab sought to develop an animal model for in vivo testing of these compounds. They have generated a mouse model carrying the most common PPT1 nonsense mutation found in the INCL patients in this country. Dr. Mukherjee received his Ph.D. from the University of Utah in Salt Lake City, Utah and underwent postdoctoral training in Human Genetics at Columbia University College of Physicians and Surgeons in New York City. He then served as an Assistant Professor of Pediatrics and Human Genetics at the State University of New York at Buffalo School of Medicine and Dentistry for four years, following which he became a medical student at the same university and received his M.D. degree. He obtained postgraduate training in Internal Medicine and after that joined the Biochemical and Developmental Genetics Section of the NICHD as a Clinical Associate. Subsequently, he joined the US Public Health Service as a Medical Officer and was promoted to the rank of Medical Director (Captain) in the USPHS. He was elected a Fellow of the Medical Sciences Section of the American Association for the Advancement of Science for his scientific achievements. He is also a member of the American Society of Biochemistry and Molecular Biology and the American Human Genetics Society. Dr. Mukherjee has received numerous honors and awards, including a USPHS Commendation Medal and a Lifetime Achievement Award from his Medical School Alumni Association. Anil B. Mukherjee, M.D., Ph.D., is a Senior Investigator and Head of the Section on Developmental Genetics, PEMG, NICHD. This Section conducts both laboratory and clinical investigations. The basic research is conducted to understand the molecular mechanism(s) of heritable neurodegenerative lysosomal storage disorders that mostly affect children. Current research focuses primarily on infantile neuronal ceroid lipofuscinosis (INCL) and juvenile NCL (JNCL), both devastating neurodegenerative storage diseases caused by mutations in the CLN1 and CLN3 genes, respectively, cause INCL and JNCL. The CLN1 gene encodes palmitoyl-protein thioesterase-1 (PPT1) and the CLN3 gene encodes a protein of 438 amino acids also called batenin. The biological function of this protein remains unclear. The laboratory research of Dr. Mukherjee and his colleagues uncovered that PPT1-deficiency leads endoplasmic reticulum and oxidative stress, which triggers unfolded protein response mediating neuronal death by apoptosis. A few years ago, researchers in this section screened many small molecules that functionally mimic PPT1. Based on results of their laboratory investigations, the Section was awarded the first NICHD “bench-to-bedside award” to conduct a clinical trial to determine if a combined regimen of Cystagon™ (cysteamine bitartrate) and Mucomyst® (N-acetylcysteine) is beneficial for patients with INCL. This study has recently been completed and the results published in Lancet Neurology. More recently, efforts to identify and characterize non-toxic small molecules, which mimic PPT1 activity, led to the discovery of N-tert (Butyl) hydroxylamine (NtBuHA), which protects neurons and extend the lifespan of Cln1-/- mice, a reliable animal model of INCL. Since many INCL patients in the US carry non-sense mutations in the CLN1 gene and increasingly, nonsense-suppressing small molecules are being developed, Mukherjee lab sought to develop an animal model for in vivo testing of these compounds. They have generated a mouse model carrying the most common PPT1 nonsense mutation found in the INCL patients in this country. Dr. Mukherjee received his Ph.D. from the University of Utah in Salt Lake City, Utah and underwent postdoctoral training in Human Genetics at Columbia University College of Physicians and Surgeons in New York City. He then served as an Assistant Professor of Pediatrics and Human Genetics at the State University of New York at Buffalo School of Medicine and Dentistry for four years, following which he became a medical student at the same university and received his M.D. degree. He obtained postgraduate training in Internal Medicine and after that joined the Biochemical and Developmental Genetics Section of the NICHD as a Clinical Associate. Subsequently, he joined the US Public Health Service as a Medical Officer and was promoted to the rank of Medical Director (Captain) in the USPHS. He was elected a Fellow of the Medical Sciences Section of the American Association for the Advancement of Science for his scientific achievements. He is also a member of the American Society of Biochemistry and Molecular Biology, the American Human Genetics Society and Society for Neuroscience. Dr. Mukherjee has received numerous honors and awards, including a USPHS Commendation Medal and a Lifetime Achievement Award from his Medical School Alumni Association.
Selected Publications
- Mukherjee AB, Appu AP, Sadhukhan T, Casey S, Mondal A, Zhang Z, Bagh MB. Emerging new roles of the lysosome and neuronal ceroid lipofuscinoses. Mol Neurodegener. 2019;14(1):4.
- Bagh MB, Peng S, Chandra G, Zhang Z, Singh SP, Pattabiraman N, Liu A, Mukherjee AB. Misrouting of v-ATPase subunit V0a1 dysregulates lysosomal acidification in a neurodegenerative lysosomal storage disease model. Nat Commun. 2017;8:14612.
- Sarkar C, Chandra G, Peng S, Zhang Z, Liu A, Mukherjee AB. Neuroprotection and lifespan extension in Ppt1(-/-) mice by NtBuHA: therapeutic implications for INCL. Nat Neurosci. 2013;16(11):1608-17.
- Levin SW, Baker EH, Zein WM, Zhang Z, Quezado ZM, Miao N, Gropman A, Griffin KJ, Bianconi S, Chandra G, Khan OI, Caruso RC, Liu A, Mukherjee AB. Oral cysteamine bitartrate and N-acetylcysteine for patients with infantile neuronal ceroid lipofuscinosis: a pilot study. Lancet Neurol. 2014;13(8):777-87.
- Appu AP, Bagh MB, Plavelil N, Mondal A, Sadhukhan T, Singh SP, Perkins NJ, Liu A, Mukherjee AB. Niemann Pick C1 mistargeting disrupts lysosomal cholesterol homeostasis contributing to neurodegeneration in a Batten disease model. Sci Adv. 2025;11(19):eadr5703.
Related Scientific Focus Areas


Molecular Biology and Biochemistry
View additional Principal Investigators in Molecular Biology and Biochemistry


This page was last updated on Monday, November 4, 2024