
Sushil Gopal Rane, Ph.D.
Senior Investigator
Integrative Cellular Metabolism Section, Diabetes, Endocrinology, & Obesity Branch
NIDDK
Research Topics
Research Goal
The overarching research goal of the Rane laboratory is to understand how growth and developmental processes of organs tasked with maintaining energy balance affects systemic glucose homeostasis. Observations will enable an integrated view of multi-organ communication that underlies normal glucose homeostasis, and its derangement in metabolic disease.
Current Research
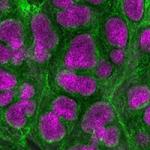
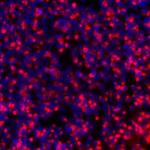
Our research is based on the central paradigm that optimal cellular growth and developmental processes are integral to lifelong systemic glucose homeostasis. Energy balance is achieved via both unique and integrative actions of multiple organ systems, necessitating a harmonious interrelationship amongst diverse organs. Indeed, dysfunction in one or more organs disturbs this delicate homeostatic balance to initiate and propagate metabolic disease. Our research is focused on understanding the unique and integrated mechanisms that enable normal glucose homeostasis as well as those that disrupt this intricate regulation. We base our research hypotheses on two inter-related themes. First, we examine the cell-specific mechanisms that underlie normal glucose homeostasis. Second, we study how the various organs, via those unique cell types, communicate to achieve metabolic harmony. To this end, we employ advanced genetic tools and techniques to understand the organization of the interorgan network tasked with maintenance of glucose homeostasis.
Applying our Research
Diabetes and obesity are global epidemics. Disease progression involves multi-organ dysfunction; thus, our findings will set the stage to help better our collective understanding of disease pathogenesis, with the potential to aid in the development of rational therapies.
Need for Further Study
Diabetes is a multiorgan malady. An integrated molecular picture of multi-organ communication and collaboration is needed to enable a better view into diabetes pathogenesis.
Biography
- Senior Investigator, NIDDK, NIH, 2012–Present
- Investigator, NIDDK, NIH, 2006–2012
- NCI Scholar, NCI, NIH, 2001–2006
- Fellow, Bristol-Myers Squibb Pharmaceutical Research Institute, 1997–1999
- Ph.D., Temple University School of Medicine, 1996
Selected Publications
- Bahn YJ, Wang Y, Dagur P, Scott N, Cero C, Long KT, Nguyen N, Cypess AM, Rane SG. TGF-β antagonism synergizes with PPARγ agonism to reduce fibrosis and enhance beige adipogenesis. Mol Metab. 2024;90:102054.
- Bahn YJ, Yadav H, Piaggi P, Abel BS, Gavrilova O, Springer DA, Papazoglou I, Zerfas PM, Skarulis MC, McPherron AC, Rane SG. CDK4-E2F3 signals enhance oxidative skeletal muscle fiber numbers and function to affect myogenesis and metabolism. J Clin Invest. 2023;133(13).
- Papazoglou I, Lee JH, Cui Z, Li C, Fulgenzi G, Bahn YJ, Staniszewska-Goraczniak HM, Piñol RA, Hogue IB, Enquist LW, Krashes MJ, Rane SG. A distinct hypothalamus-to-β cell circuit modulates insulin secretion. Cell Metab. 2022;34(2):285-298.e7.
- Wankhade UD, Lee JH, Dagur PK, Yadav H, Shen M, Chen W, Kulkarni AB, McCoy JP, Finkel T, Cypess AM, Rane SG. TGF-β receptor 1 regulates progenitors that promote browning of white fat. Mol Metab. 2018;16:160-171.
- Yadav H, Quijano C, Kamaraju AK, Gavrilova O, Malek R, Chen W, Zerfas P, Zhigang D, Wright EC, Stuelten C, Sun P, Lonning S, Skarulis M, Sumner AE, Finkel T, Rane SG. Protection from obesity and diabetes by blockade of TGF-β/Smad3 signaling. Cell Metab. 2011;14(1):67-79.
Related Scientific Focus Areas


Molecular Biology and Biochemistry
View additional Principal Investigators in Molecular Biology and Biochemistry

This page was last updated on Thursday, August 7, 2025