
Karen M. Frank, M.D., Ph.D.
Senior Clinician
Department of Laboratory Medicine
NIH Clinical Center
Research Topics
The Microbiology Service is a CAP-accredited 7,000 square foot laboratory, offering tests that cover all areas of microbiology, including bacteriology, mycology, parasitology, mycobacteriology, and virology. We provide testing for many NIH institute research programs and we therefore have state-of-the-art instrumentation, including an extensive molecular diagnostics section and a BSL3 level facility. The laboratory staff have consistently published peer-reviewed studies for many years. This laboratory was one of the leading laboratories in the United States to investigate the use of MALDI-TOF technology for organism identification and to integrate the technology into the routine daily workflow. We have more than 26 full-time microbiology staff, primarily licensed medical technologists, as well as four senior level microbiology staff positions to oversee all of the sections of the laboratory. The Clinical Center serves as a medical center only for patients enrolled in clinical trials, and because of this unique mission, the patients enrolled come from locations throughout the world, some with very rare disorders, and many of the patients are very immunocompromised. Therefore, we recover a variety of organisms, some of which are not routinely isolated in many hospital settings. The senior staff in the microbiology laboratory meets daily with the infectious diseases physicians and has routine interactions with the scientists leading the clinical trials, providing a great environment for further investigation of antibacterial resistance. Collaborative research is conducted on campus with investigators from multiple NIH institutes.
Research Interests
Staphylococcus aureus
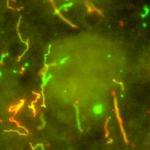
Dr. Frank's research collaboration with Dr. Julie Bubeck-Wardenburg in the Departments of Pediatrics and Microbiology at the University of Chicago focused on the pathogenesis of Staphylococcus aureus pneumonia. Pneumonia due to Staphylococcus aureus causes significant morbidity and mortality in both children and adults. Although Staphylococcus aureus is known to have a number of virulence factors, the essential factors involved in lower respiratory tract disease are not yet completely understood. The alpha-hemolysin of Staphylococcus aureus has been identified through animal models of pneumonia as one of the critical virulence factors for lung injury.
Using microarray analysis of murine lung RNA, we examined the response of the host to a virulent Staphylococcal strain compared to a strain deficient in the alpha-toxin. We determined that the cellular immune response to infection was characterized by a prominent TH17 response to the wild-type pathogen. Investigation of the host-pathogen interaction and the pathogenesis of Staphylococcal lung injury will contribute to programs aimed at the development of novel therapeutic approaches for Staphylococcal disease.
Resistant Gram Negative Bacteria
Antibiotic-resistant bacteria cause significant morbidity and mortality in hospitalized patients, causing the Centers for Disease Control and Prevention to list carbapenem-resistant bacteria as a urgent threat requiring attention by the medical community.
Investigators in the National Human Genome Research Institute and the Clinical Center have used advanced DNA sequencing methods to characterize carbapenem-resistant Enterobacteriaceae in hospitalized patients. They tracked a cluster of infections in hospitalized patients, then more recently, we conducted a two year follow-up study to understand the possible spread of the resistant genes between bacteria on plasmids, the genetic material which encodes antibiotic resistant genes in these bacteria.
Advanced sequencing is a valuable technique to aid the infection control team in learning how to control the spread of multi-drug resistant bacteria between critically ill patients at the NIH Clinical Center as a model for healthcare systems. Improved understanding of the genetic basis of antibiotic resistant bacteria guides further strategies to rein in antibiotic resistance and focus experiments directed toward improved treatment for these serious infections.
To further investigate the mechanisms used by bacteria to spread resistance, we examined the frequency of horizontal gene transfer among species, using bacterial isolates from two hospitals. Most conjugation studies use a lab strain of E. coli, typically under narrow conditions. Given that conjugation is influenced by multiple factors, we sought to perform a systematic analysis of blaKPC encoding plasmids transfer into multiple species.
The efficiency of conjugation into Enterobacteriaceae patient isolates and a common lab cloning E. coli strain ranged widely from high rates of 10-2 or 10-3 CFU transconjugants/CFU recipients to undetectable, without a clear correlation with the pattern of spread suggested during two hospital outbreaks. In vitro models may not faithfully predict plasmid mobilization until we better understand the most important variables affecting conjugation efficiency. Additional studies will be valuable in assessing the role of conjugation in the worldwide spread of resistance as compared to other factors contributing to the success of epidemic clones.
Biography
Dr. Frank completed her M.D. and Ph.D. in Biochemistry at the University of Pennsylvania. She completed a Clinical Pathology Residency at the Brigham & Women's Hospital. During her postdoctoral research fellowship in Immunology, she focused on V(D)J recombination in developing lymphocytes in the HHMI laboratory of Dr. Fred Alt at the Boston Children's Hospital. As a faculty member, her studies included DNA repair mechanisms relevant to both cancer and immunology, followed by microbiological investigations of Staphylococcus aureus and Enterobacteriaceae.
Selected Publications
- Decker BK, Lau AF, Dekker JP, Spalding CD, Sinaii N, Conlan S, Henderson DK, Segre JA, Frank KM, Palmore TN. Healthcare personnel intestinal colonization with multidrug-resistant organisms. Clin Microbiol Infect. 2018;24(1):82.e1-82.e4.
- Conlan S, Park M, Deming C, Thomas PJ, Young AC, Coleman H, Sison C, NISC Comparative Sequencing Program., Weingarten RA, Lau AF, Dekker JP, Palmore TN, Frank KM, Segre JA. Plasmid Dynamics in KPC-Positive Klebsiella pneumoniae during Long-Term Patient Colonization. mBio. 2016;7(3).
- Hardiman CA, Weingarten RA, Conlan S, Khil P, Dekker JP, Mathers AJ, Sheppard AE, Segre JA, Frank KM. Horizontal Transfer of Carbapenemase-Encoding Plasmids and Comparison with Hospital Epidemiology Data. Antimicrob Agents Chemother. 2016;60(8):4910-9.
- Weingarten RA, Johnson RC, Conlan S, Ramsburg AM, Dekker JP, Lau AF, Khil P, Odom RT, Deming C, Park M, Thomas PJ, NISC Comparative Sequencing Program., Henderson DK, Palmore TN, Segre JA, Frank KM. Genomic Analysis of Hospital Plumbing Reveals Diverse Reservoir of Bacterial Plasmids Conferring Carbapenem Resistance. mBio. 2018;9(1).
- Conlan S, Thomas PJ, Deming C, Park M, Lau AF, Dekker JP, Snitkin ES, Clark TA, Luong K, Song Y, Tsai YC, Boitano M, Dayal J, Brooks SY, Schmidt B, Young AC, Thomas JW, Bouffard GG, Blakesley RW, NISC Comparative Sequencing Program., Mullikin JC, Korlach J, Henderson DK, Frank KM, Palmore TN, Segre JA. Single-molecule sequencing to track plasmid diversity of hospital-associated carbapenemase-producing Enterobacteriaceae. Sci Transl Med. 2014;6(254):254ra126.
Related Scientific Focus Areas
Microbiology and Infectious Diseases
View additional Principal Investigators in Microbiology and Infectious Diseases

This page was last updated on Tuesday, February 11, 2025