
Theo Heller, M.D.
Senior Investigator
Translational Hepatology Section, Liver Diseases Branch
NIDDK
Research Topics
Liver disease presents a unique confluence of many disciplines, in both the basic science and clinical realms. Additionally, there are many unanswered questions in terms of basic hepatic biology and the development of liver disease. Our laboratory is interested in testing hypotheses in clinical situations that can be translated into laboratory projects, which in turn might lead to fundamental biologic insights and improved disease management. A philosophical approach is that clinical observations can sometimes best be explained at the bench and that human disease investigation is in many ways better than a model—it is a direct study of authentic biology. It is believed that human disease is a window into biology and that by studying diseases, some rare, derived concepts may be extrapolated to a far broader understanding of biologic principles.
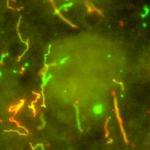
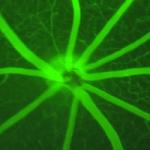
The laboratory focus is on the intersection of the innate immune system and hepatic damage and repair. The clinical focus is on noncirrhotic portal hypertension, including nodular regenerative hyperplasia. Patients with chronic granulomatous disease, sickle cell disease, Turner syndrome, and sporadic nodular regenerative hyperplasia drive both the laboratory and clinical research. These projects are the result of significant collaborations with multiple other investigators. Additionally, we have a long-standing interest in hepatitis D, acute hepatitis C, and congenital hepatic fibrosis.
All of the work is carried out with the direct mentorship of T. Jake Liang, M.D., the branch chief. The clinical projects also benefit from the involvement and direction of Jay Hoofnagle, M.D.
Current Research
A variety of clinical and laboratory researchers are involved in the study of liver disease, as many questions remain unanswered about hepatic—liver-related— biology and how liver disease begins.
Our laboratory tests hypotheses, in clinical situations, with patients. The results can then be adapted into laboratory projects that may lead to fundamental biologic insights and better disease management. We believe it is often better to study human disease through real-life clinical observations than through models.
Human disease is a window into biology. Thus, by studying diseases—some rare—researchers can use the concepts learned to gain a better understanding of far broader biologic principles.
Our laboratory focuses on the connections between the innate immune system and liver-related damage and repair. The clinical focus is on noncirrhotic portal hypertension, which is when a person’s blood pressure rises above normal levels in the hepatic circulation of the liver for other reasons than the liver disease called cirrhosis. We also study patients with chronic granulomatous disease, sickle cell disease, Turner syndrome, sporadic nodular regenerative hyperplasia, hepatitis D, acute hepatitis C, and congenital hepatic fibrosis.
Applying our Research
Due to our research in this area, fewer people will die of liver disease, a disease that disproportionately affects people during their most productive working years.
Biography
- Hepatology Fellowship, LDB, NIDDK, NIH, 2003
- Gastroenterology and Hepatology Fellowship, University of Maryland Medical Systems, 2000
- Postdoctoral Fellowship, Hepatitis Viruses Section, NIAID, 1997
- Internal Medicine Residency, Georgetown University Hospital, 1993
- M.D., University of the Witwatersrand, 1989
- B.S., University of Cape Town, 1983
Selected Publications
- Reshamwala PA, Kleiner DE, Heller T. Nodular regenerative hyperplasia: not all nodules are created equal. Hepatology. 2006;44(1):7-14.
- Gunay-Aygun M, Font-Montgomery E, Lukose L, Tuchman Gerstein M, Piwnica-Worms K, Choyke P, Daryanani KT, Turkbey B, Fischer R, Bernardini I, Sincan M, Zhao X, Sandler NG, Roque A, Douek DC, Graf J, Huizing M, Bryant JC, Mohan P, Gahl WA, Heller T. Characteristics of congenital hepatic fibrosis in a large cohort of patients with autosomal recessive polycystic kidney disease. Gastroenterology. 2013;144(1):112-121.e2.
- Ali RO, Quinn GM, Umarova R, Haddad JA, Zhang GY, Townsend EC, Scheuing L, Hill KL, Gewirtz M, Rampertaap S, Rosenzweig SD, Remaley AT, Han JM, Periwal V, Cai H, Walter PJ, Koh C, Levy EB, Kleiner DE, Etzion O, Heller T. Longitudinal multi-omics analyses of the gut-liver axis reveals metabolic dysregulation in hepatitis C infection and cirrhosis. Nat Microbiol. 2023;8(1):12-27.
- Sharma D, Ben Yakov G, Kapuria D, Viana Rodriguez G, Gewirtz M, Haddad J, Kleiner DE, Koh C, Bergerson JRE, Freeman AF, Heller T. Tip of the iceberg: A comprehensive review of liver disease in Inborn errors of immunity. Hepatology. 2022;76(6):1845-1861.
- Koh C, Canini L, Dahari H, Zhao X, Uprichard SL, Haynes-Williams V, Winters MA, Subramanya G, Cooper SL, Pinto P, Wolff EF, Bishop R, Ai Thanda Han M, Cotler SJ, Kleiner DE, Keskin O, Idilman R, Yurdaydin C, Glenn JS, Heller T. Oral prenylation inhibition with lonafarnib in chronic hepatitis D infection: a proof-of-concept randomised, double-blind, placebo-controlled phase 2A trial. Lancet Infect Dis. 2015;15(10):1167-1174.
Related Scientific Focus Areas

Microbiology and Infectious Diseases
View additional Principal Investigators in Microbiology and Infectious Diseases

Molecular Biology and Biochemistry
View additional Principal Investigators in Molecular Biology and Biochemistry
This page was last updated on Wednesday, January 10, 2024