Natalie Shaw, M.D., MMSc.
Senior Investigator
Clinical Research Branch / Pediatric Neuroendocrinology Group
NIEHS
Research Topics
Our group has three major research interests:
- To investigate the contributions of body weight, abnormal sleep patterns, and other environmental factors to irregular menstrual cycles in adolescent girls during the first few years after menarche (a girl's first period). While irregular menstrual cycles are a common part of female development, a subset of teens never make the critical transition to normal menstrual cycles. By investigating the physiologic and pathophysiologic underpinnings of irregular menstrual cycles in adolescent girls in the 1-2 years after their first menses, the Pediatric Neuroendocrinology Group intends to identify those girls who are at high-risk for reproductive dysfunction as adults. Girls with pathologic menstrual cycle patterns would then be encouraged to seek early treatment to prevent future hormonal and metabolic complications.
- To determine the influence of obesity on pubertal timing in girls. Over the past decade, there has been an alarming trend toward earlier breast development in girls. The contemporaneous obesity epidemic has led to speculation that obesity may be driving early puberty. However, questions remain about the validity of reports of early puberty among obese girls due to the difficulty in distinguishing fatty tissue from breast tissue by palpation in this population. The physiological basis for early puberty among obese girls is also unknown. The group has initiated the NIEHS Body Weight & Puberty Study to investigate pubertal development in obese compared with normal weight girls using more robust methods such as breast ultrasonography. Study procedures also include blood draws, DEXA (for body composition), hand x-ray (for bone age), transabdominal (pelvic) ultrasounds, and anthropometrics (height, weight, BMI, waist-hip ratio). The group is actively recruiting for this study, which is being conducted at the NIEHS Clinical Research Unit.
- To determine the genetic architecture of Bosma Arhinia Microphthalmia Syndrome, a rare syndromic form of hypogonadism. Patients with Bosma syndrome are born without an external nose (arhinia) and with small or absent eyes (microphthalmia or anophthalmia). They also don't undergo puberty and are infertile (hypogonadotropic hypogonadism). This condition is extremely rare, with only about 70 cases reported worldwide in the past century. The group is working with scientists at Harvard University, Duke University, and the University of Edinburgh to determine the genetic basis for Bosma syndrome using next generation sequencing.
Biography
Dr. Shaw received a B.S. from Cornell University, an M.D. from the State University of New York (SUNY) at Buffalo, and a Masters in Medical Sciences (MMSc) from Harvard Medical School. She completed her pediatrics residency at Children's Hospital of Pittsburgh, a pediatric endocrinology fellowship at Boston Children's Hospital, and a clinical research fellowship in the Reproductive Endocrine Unit at Massachusetts General Hospital. She is now a Lasker Clinical Research Scholar and PI of the Pediatric Neuroendocrinology Group in the Clinical Research Branch of NIEHS.
Selected Publications
- Shaw ND, Brand H, Kupchinsky ZA, Bengani H, Plummer L, Jones TI, Erdin S, Williamson KA, Rainger J, Stortchevoi A, Samocha K, Currall BB, Dunican DS, Collins RL, Willer JR, Lek A, Lek M, Nassan M, Pereira S, Kammin T, Lucente D, Silva A, Seabra CM, Chiang C, An Y, Ansari M, Rainger JK, Joss S, Smith JC, Lippincott MF, Singh SS, Patel N, Jing JW, Law JR, Ferraro N, Verloes A, Rauch A, Steindl K, Zweier M, Scheer I, Sato D, Okamoto N, Jacobsen C, Tryggestad J, Chernausek S, Schimmenti LA, Brasseur B, Cesaretti C, García-Ortiz JE, Buitrago TP, Silva OP, Hoffman JD, Mühlbauer W, Ruprecht KW, Loeys BL, Shino M, Kaindl AM, Cho CH, Morton CC, Meehan RR, van Heyningen V, Liao EC, Balasubramanian R, Hall JE, Seminara SB, Macarthur D, Moore SA, Yoshiura KI, Gusella JF, Marsh JA, Graham JM Jr, Lin AE, Katsanis N, Jones PL, Crowley WF Jr, Davis EE, FitzPatrick DR, Talkowski ME. Corrigendum: SMCHD1 mutations associated with a rare muscular dystrophy can also cause isolated arhinia and Bosma arhinia microphthalmia syndrome. Nat Genet. 2017;49(6):969.
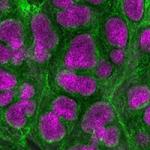
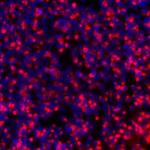
- Inoue K, Bostan H, Browne MR, Bevis OF, Bortner CD, Moore SA, Stence AA, Martin NP, Chen SH, Burkholder AB, Li JL, Shaw ND. DUX4 double whammy: The transcription factor that causes a rare muscular dystrophy also kills the precursors of the human nose. Sci Adv. 2023;9(7):eabq7744.
- Pedersen LC, Inoue K, Kim S, Perera L, Shaw ND. A ubiquitin-like domain is required for stabilizing the N-terminal ATPase module of human SMCHD1. Commun Biol. 2019;2:255.
- Ortega MT, McGrath JA, Carlson L, Flores Poccia V, Larson G, Douglas C, Sun BZ, Zhao S, Beery B, Vesper HW, Duke L, Botelho JC, Filie AC, Shaw ND. Longitudinal Investigation of Pubertal Milestones and Hormones as a Function of Body Fat in Girls. J Clin Endocrinol Metab. 2021;106(6):1668-1683.
- Yang S, Zhang L, Khan K, Travers J, Huang R, Jovanovic VM, Veeramachaneni R, Sakamuru S, Tristan CA, Davis EE, Klumpp-Thomas C, Witt KL, Simeonov A, Shaw ND, Xia M. Identification of Environmental Compounds That May Trigger Early Female Puberty by Activating Human GnRHR and KISS1R. Endocrinology. 2024;165(10).
Related Scientific Focus Areas
This page was last updated on Thursday, April 17, 2025