Research Topics
The immune system is designed to effectively combat pathogens while tolerating commensal organisms and harmless environmental substances. The balance struck is particularly important in the intestine, where tissues are continuously exposed to a massive number and variety of food antigens and commensal bacteria. The breakdown of these and other homeostatic control mechanisms results in inflammatory bowel disease (IBD), including Crohn's disease and ulcerative colitis. Although immunotherapies such as TNF inhibitors are a major advance in the treatment of IBD, many patients do not respond, indicating an unmet medical need, as well as a need for a more detailed understanding of the mucosal immunology of the gut at the molecular and cellular levels. Furthermore, the nature and regulation of immune responses to commensal bacteria and intestinal pathogens, as well as to oral vaccines that are known to have decreased efficacy in underdeveloped areas of the world, are poorly understood.
The MIS research program seeks to understand the mechanisms by which homeostatic immunity to commensal microbes is controlled and effector immune responses to pathogens are induced as well as how the composition of commensal bacteria effects homeostasis and immunity to pathogens and vaccine in the intestine.
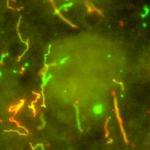
Intestinal dendritic cell and macrophage biology
A major goal of the MIS is to define the development and functions of innate myeloid cells in the intestine. Using state-of-the-art cellular, molecular, genetic, and imaging technologies, we are comprehensively defining conventional dendritic cell (cDC) and macrophage (MP) populations in the intestine and delineating their functions during homeostasis and following experimental intestinal inflammation in mouse models of IBD. The program scope also includes investigation of mucosal immunity using intestinal samples from patients with Crohn's disease and ulcerative colitis.
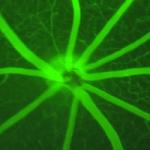
Innate and adaptive immunity to commensals, pathogens, and oral vaccines
A second related major focus of the MIS is to understand how regulatory and adaptive T and B cells are induced in the intestine. Using scmRNA-seq and other technologies, we are elucidating the mechanisms by which SIgA and T cell responses are induced in the intestine to commensal bacteria and mucosal pathogens, and studying how the composition of the microbiome affects immune responses to oral vaccines.
Biography
Dr. Kelsall received his B.A. in human biology from Stanford University in 1982. In 1986, he earned his M.D. from Case Western Reserve University School of Medicine. He did postdoctoral training in internal medicine at The New York Hospital-Cornell Medical Center from 1986 to 1989 and in infectious diseases at the University of Virginia Medical Center from 1989 to 1992.
In 1992, Dr. Kelsall came to the National Institutes of Health, completed fellowship training in mucosal immunology in 1996, and became a senior investigator in 2003. His research focuses on the regulation of immune responses in the intestine, in particular the role that unique intestinal dendritic cell and macrophage populations play in the induction of immunity to intestinal viral pathogens and mucosal vaccines and in the pathogenesis of inflammatory bowel disease.
Selected Publications
- Rivollier A, He J, Kole A, Valatas V, Kelsall BL. Inflammation switches the differentiation program of Ly6Chi monocytes from antiinflammatory macrophages to inflammatory dendritic cells in the colon. J Exp Med. 2012;209(1):139-55.
- Kang B, Alvarado LJ, Kim T, Lehmann ML, Cho H, He J, Li P, Kim BH, Larochelle A, Kelsall BL. Commensal microbiota drive the functional diversification of colon macrophages. Mucosal Immunol. 2020;13(2):216-229.
- Iwasaki A, Kelsall BL. Freshly isolated Peyer's patch, but not spleen, dendritic cells produce interleukin 10 and induce the differentiation of T helper type 2 cells. J Exp Med. 1999;190(2):229-39.
- Johansson C, Wetzel JD, He J, Mikacenic C, Dermody TS, Kelsall BL. Type I interferons produced by hematopoietic cells protect mice against lethal infection by mammalian reovirus. J Exp Med. 2007;204(6):1349-58.
- Cho H, Jaime H, de Oliveira RP, Kang B, Spolski R, Vaziri T, Myers TG, Thovarai V, Shen Z, Fox JG, Leonard WJ, Kelsall BL. Defective IgA response to atypical intestinal commensals in IL-21 receptor deficiency reshapes immune cell homeostasis and mucosal immunity. Mucosal Immunol. 2019;12(1):85-96.
Related Scientific Focus Areas

Microbiology and Infectious Diseases
View additional Principal Investigators in Microbiology and Infectious Diseases


This page was last updated on Wednesday, May 22, 2024