A Two-year Clinical Research Odyssey
William Gahl searches for answers to some of the most confounding undiagnosed diseases.
The sets of inches-thick medical records arrive in boxes and padded envelopes and accumulate around the desk of William Gahl, director of the NIH Undiagnosed Diseases Program (UDP). The two- and three-foot stacks represent cases that need to be reviewed and sorted, mostly by Gahl, who is also the clinical director at the National Human Genome Research Institute (NHGRI).
They are among the hundreds of such records sent by doctors and their patients who are hoping to participate in the UDP. Gahl, who is known for his affable manner and wry sense of humor among his National Institutes of Health (NIH) intramural colleagues and patients, is filled with concern as he reads each desperate case. The influx has been unprecedented and Gahl knows that he can’t accept all these people into this new clinical research program.

A three-year-old patient with no diagnosis for his developmental disorder undergoes a neurological exam
“As doctors, we feel deep compassion for patients who have been without hope because they are sick and no one has been able to help them. For some, this program offers real hope and maybe even relief,” said Gahl. “A principal mission of UDP, however, is the discovery of new diseases and variations of known diseases.”
The NIH has been bringing sick people to its main campus for decades. Usually, people are recruited to participate in clinical studies that have a defined focus such as the study of a particular cancer. When they volunteer to test new procedures or treatments, not only may they get help for themselves but they also contribute to the overall understanding of the natural history of disease.
But UDP is different. Since 2008, this trans-NIH initiative has embraced a broader view. Instead of focusing on a single disease, UDP tackles the hardest-to-diagnose disorders relying on a spectrum of NIH specialists—in endocrinology, immunology, oncology, dermatology, dentistry, cardiology, genetics, and other areas—to apply their expertise and come up with insights about each case. A unified diagnosis is the optimal but often elusive endpoint of their efforts.
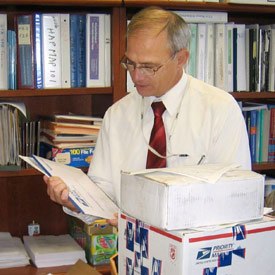
UDP Director William Gahl receives medical records from hopeful applicants
“We expected to diagnose maybe 10 or 15 percent of the patients that we admitted, and we have achieved roughly that,” said Gahl.
In the two years that the program has been operating, the UDP has responded to about 3,000 inquiries, received nearly 1,200 medical records, and accepted some 280 cases from all corners of the country. To be considered for the program, a patient must be referred by a physician and provide all medical records and diagnostic test results requested by the NIH. Patients who meet the program’s criteria are then asked to undergo an additional weeklong evaluation during a visit to the NIH Clinical Center.
Genetics plays a unique role in the UDP. “Before coming to the NIH, our patients have been to center throughout the country and have gotten the standard genetic tests that largely focus on a particular symptom,” said Gahl. We consider those tests as a starting point.”
Gahl described a family of five adult siblings who all had the same problem affecting the large vessels in their legs, leading to difficulties in walking. Their parents were fine. Using a million-SNP (single-nucleotide polymorphism) array developed by the NHGRI, Gahl and his team found a single gene in which the siblings all had mutations in both alleles, where their parents did not. “We realized that this is, in fact, a new disease.”
In some cases, UDP can not only make a diagnosis, but also provide treatment or appropriate referrals. “But even when there is no treatment, simply having our diagnosis can be helpful,” said Gahl. “Patients find it comforting to have some certitude in their lives, some expectation, some prognosis that’s associated with a diagnosis.”
William Gahl, M.D., Ph.D., is Clinical Director of the National Human Genome Research Institute (NHGRI) and Senior Investigator in the Medical Genetics Branch.
Adapted from an article that appeared in The NIH Catalyst Volume 18 Issue 5, September-October 2010, by Raymond MacDougall
Further reading:
This page was last updated on Wednesday, May 24, 2023