FDA-approved drug shows promise in lab models for blinding childhood disease
Strategy may speed delivery of therapeutic options relative to time it would take to develop gene therapies
A National Institutes of Health team has identified a compound already approved by the U.S. Food and Drug Administration that keeps light-sensitive photoreceptors alive in three models of Leber congenital amaurosis type 10 (LCA 10), an inherited retinal ciliopathy disease that often results in severe visual impairment or blindness in early childhood.
LCA 10 is caused by mutations of the cilia-centrosomal gene (CEP290). Such mutations account for 20% to 25% of all LCA — more than any other gene. In addition to LCA, CEP290 mutations can cause multiple syndromic diseases involving a range of organ systems.
Using a mouse model of LCA10 and two types of lab-created tissues from stem cells known as organoids, the team screened more than 6,000 FDA-approved compounds to identify ones that promoted survival of photoreceptors, the types of cells that die in LCA, leading to vision loss. The high-throughput screening identified five potential drug candidates, including Reserpine, an old medication previously used to treat high blood pressure.
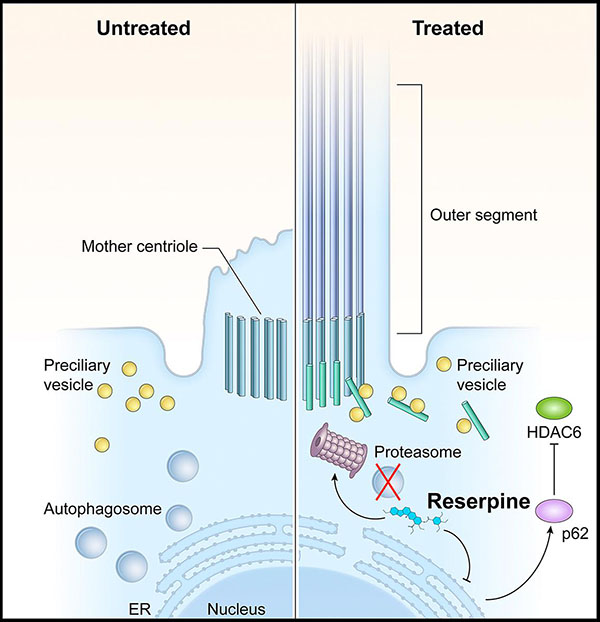
In LCA10, CEP290 mutations lead to defects in the photoreceptor outer segment. Consequently, the building blocks of the primary cilium accumulate in the photoreceptors, which activates autophagy (shown left, untreated). Reserpine restores the balance between autophagy and the ubiquitin-proteasome system histone deacetylase 6 and improves primary cilium assembly.
This page was last updated on Wednesday, March 29, 2023