Research Topics
The research program of GIS includes both clinical trials and basic bench research. Clinical trials include studies of gene therapy using ex vivo transduction of autologous CD34+ hematopoietic stem cells, as well as studies of allogeneic transplantation using matched-sibling donor or matched-unrelated donor (MUD) hematopoietic stem cell grafts with sub-ablative marrow conditioning plus alloimmune tolerance induction regimens. Elizabeth Kang, M.D., staff clinician and chief of the hematotherapeutics unit of GIS, has a major role in development and implementation of clinical trials in GIS. Suk See De Ravin, M.D., staff clinician, has a major role in development and conduct of clinical trials to treat autoimmune and inflammation problems affecting patients with immune deficiencies under study in the GIS.
The GIS gene therapy program has a particular focus at the bench and in the clinic on development of gene transfer treatments for X-linked chronic granulomatous disease (CGD) and X-linked severe combined immune deficiency (X-SCID). Both Dr. Kang and Dr. De Ravin are involved in the conduct of clinical trials of gene therapy for these disorders. GIS also collaborates closely with investigators in the National Cancer Institute who are working toward development of gene therapy for leukocyte adhesion deficiency (LAD).
The bone marrow transplant program is focused on developing improved methods of transplant to treat primary immune deficiencies and includes hematopoietic stem cell transplant using bone marrow, mobilized peripheral blood stem cells, or cord blood from either an HLA-matched sibling or an unrelated donor. Because hematopoietic stem cell transplantation carries a significant risk of causing graft versus host disease (GVHD), the GIS transplant program includes clinical protocols and bench research to develop methods and treatments to prevent or treat acute and chronic GVHD.
Basic laboratory work in GIS is focused on the biology of human hematopoietic stem cells (HSCs) and induced pluripotent stem cells (iPSCs); the development of new gene transfer vectors and associated methods for gene transfer into HSCs and iPSCs; and the delineation of immune factors affecting allogeneic transplantation, including prevention and treatment of GVHD.
Work on stem cells is focused on the biology of hematopoietic progenitor/stem cells in humans (the CD34+ cell) and in mice (the Sca-1+ cell), including studies of the regulation of engraftment of stem cells in the marrow through CXCR4 receptor/SDF-1 ligand interactions. There is also an interest in delineating the biochemical abnormalities seen with the mutant forms of CXCR4 that cause the myelokathexis, neutopenia, and susceptibility to human papilloma-virus infections characteristic of the immune deficiency known as WHIM syndrome.
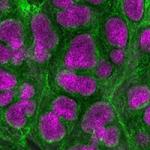
GIS also has a basic and pre-clinical program of study of induced pluripotent stem cells (iPSC). This work is focused on development of iPSC from patients with immune deficiencies under study in GIS. Recent work from GIS has been reported regarding the development of iPSC from patients with X-linked CGD, the genetic correction of these patient iPSC, and demonstration that neutrophils with normal oxidant production function can be differentiated from these X-linked CGD patient iPSC that have been genetically corrected.
Basic work on gene therapy vectors has a particular focus on the development of self-inactivating, insulated, lentivirus vectors, which may have improved performance and safety characteristics. Current pre-clinical work is aimed at getting lentivectors into the clinic in the near term to treat X-CGD and X-SCID. The laboratory is also working to develop zinc finger nuclease technology to achieve specifically targeted gene correction in patient hematopoietic stem cells and in patient-derived iPSC.
Basic work on GVHD is focused on delineating mechanisms by which tolerance is developed after bone marrow transplant, as well as developing methods to enhance development of tolerance after transplant using rapamycin or other tolerance-inducing agents.
Biography
Dr. Malech received his medical degree from Yale University in New Haven, Connecticut, in 1972. He completed clinical residency training at the University of Pennsylvania in Philadelphia, followed by basic research postdoctoral fellowship training at the National Institutes of Health (NIH) in Bethesda, Maryland. After then completing clinical fellowship training in infectious diseases at Yale University, he remained at Yale as assistant and then associate professor until 1986. In 1986, he returned to NIH as a senior investigator in NIAID. He is currently chief of the Laboratory of Host Defenses (LHD). Dr. Malech’s research and clinical program within LHD is the Genetic Immunotherapy Section (GIS).
The mission of GIS is the development of gene therapy and hematopoietic stem cell transplantation approaches to the treatment of a variety of inherited primary immune deficiencies. Associated with that mission is the diagnosis and treatment of the infections, inflammation, autoimmunity, pulmonary dysfunction, and growth failure that may complicate management of a number of primary immune deficiencies.
Selected Publications
- Kohn DB, Booth C, Shaw KL, Xu-Bayford J, Garabedian E, Trevisan V, Carbonaro-Sarracino DA, Soni K, Terrazas D, Snell K, Ikeda A, Leon-Rico D, Moore TB, Buckland KF, Shah AJ, Gilmour KC, De Oliveira S, Rivat C, Crooks GM, Izotova N, Tse J, Adams S, Shupien S, Ricketts H, Davila A, Uzowuru C, Icreverzi A, Barman P, Campo Fernandez B, Hollis RP, Coronel M, Yu A, Chun KM, Casas CE, Zhang R, Arduini S, Lynn F, Kudari M, Spezzi A, Zahn M, Heimke R, Labik I, Parrott R, Buckley RH, Reeves L, Cornetta K, Sokolic R, Hershfield M, Schmidt M, Candotti F, Malech HL, Thrasher AJ, Gaspar HB. Autologous Ex Vivo Lentiviral Gene Therapy for Adenosine Deaminase Deficiency. N Engl J Med. 2021;384(21):2002-2013.
- Cowan MJ, Yu J, Facchino J, Fraser-Browne C, Sanford U, Kawahara M, Dara J, Long-Boyle J, Oh J, Chan W, Chag S, Broderick L, Chellapandian D, Decaluwe H, Golski C, Hu D, Kuo CY, Miller HK, Petrovic A, Currier R, Hilton JF, Punwani D, Dvorak CC, Malech HL, McIvor RS, Puck JM. Lentiviral Gene Therapy for Artemis-Deficient SCID. N Engl J Med. 2022;387(25):2344-2355.
- Kohn DB, Booth C, Kang EM, Pai SY, Shaw KL, Santilli G, Armant M, Buckland KF, Choi U, De Ravin SS, Dorsey MJ, Kuo CY, Leon-Rico D, Rivat C, Izotova N, Gilmour K, Snell K, Dip JX, Darwish J, Morris EC, Terrazas D, Wang LD, Bauser CA, Paprotka T, Kuhns DB, Gregg J, Raymond HE, Everett JK, Honnet G, Biasco L, Newburger PE, Bushman FD, Grez M, Gaspar HB, Williams DA, Malech HL, Galy A, Thrasher AJ, Net4CGD consortium. Lentiviral gene therapy for X-linked chronic granulomatous disease. Nat Med. 2020;26(2):200-206.
- Mamcarz E, Zhou S, Lockey T, Abdelsamed H, Cross SJ, Kang G, Ma Z, Condori J, Dowdy J, Triplett B, Li C, Maron G, Aldave Becerra JC, Church JA, Dokmeci E, Love JT, da Matta Ain AC, van der Watt H, Tang X, Janssen W, Ryu BY, De Ravin SS, Weiss MJ, Youngblood B, Long-Boyle JR, Gottschalk S, Meagher MM, Malech HL, Puck JM, Cowan MJ, Sorrentino BP. Lentiviral Gene Therapy Combined with Low-Dose Busulfan in Infants with SCID-X1. N Engl J Med. 2019;380(16):1525-1534.
- De Ravin SS, Liu S, Sweeney CL, Brault J, Whiting-Theobald N, Ma M, Liu T, Choi U, Lee J, O'Brien SA, Quackenbush P, Estwick T, Karra A, Docking E, Kwatemaa N, Guo S, Su L, Sun Z, Zhou S, Puck J, Cowan MJ, Notarangelo LD, Kang E, Malech HL, Wu X. Lentivector cryptic splicing mediates increase in CD34+ clones expressing truncated HMGA2 in human X-linked severe combined immunodeficiency. Nat Commun. 2022;13(1):3710.
Related Scientific Focus Areas
This page was last updated on Saturday, August 26, 2023