Research Topics
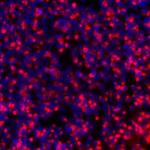
Our research interests span basic laboratory studies through pioneering clinical trials focusing on stem cell biology and hematopoiesis—the development and differentiation of bone marrow stem cells into multiple types of blood cells. Hematopoiesis occurs throughout life, and dysfunction of these processes can result in bone marrow failure or leukemia. We utilize cutting edge molecular technologies such as genetic barcoding and single cell gene expression analyses to understand the “family tree” linking stem cells to their daughter cells and eventually to mature circulating blood cells, in both health and disease. For over thirty years, our research group has utilized the rhesus macaque transplantation model to study hematopoiesis and the immune system. This model provides unique predictive insights into human hematopoiesis and blood diseases. Our studies have provided insights into stem cell frequency, lifespan, aging, geographic location, and differentiation. Recently we provided the first direct evidence for self-renewal and long-term persistence of mature natural killer cells, explaining aspects of natural killer cell memory and providing insights into dynamics of these cells following infections or as therapies to fight cancer.
We have also been engaged in more than three decades of efforts to design, optimize and utilize methods to genetically modify or correct hematopoietic stem cells, with direct translation to human gene therapies. We have focused on understanding and improving the safety and effectiveness of a variety of gene transfer vectors that integrate into the genome of hematopoietic stem cells. The rhesus macaque model has been of great utility for assessment of the safety and efficacy of novel gene and cell therapies. These translational studies have provided critical information to improve clinical gene therapies targeting blood diseases such as inherited immunodeficiencies and sickle cell anemia. We have also investigated gene editing technologies, such as CRISPR/Cas9, to correct or modify the genome at specific gene targets, creating macaque models of human hematopoietic stem cell aging and marrow failure disorders, and using gene editing to overcome potential toxicities of CAR-T cells directed against forms of leukemia.
We have expanded our focus to other types of stem cells, particularly induced pluripotent stem cells (iPSC). We were the first to derive rhesus macaque iPSC and have gone on to use the rhesus iPSC model to develop safe and effective approaches for tissue and organ regeneration, particularly focused on the heart, and on methodologies to track cells in vivo long-term following administration, crucial information for optimizing safety and efficacy of clinical cell therapy products.
Clinically, we have led the clinical development of approaches to stimulate human hematopoietic stem cells in vivo, most notably in patients with severe refractory aplastic anemia. The small molecule oral drug eltrombopag was found to improve blood counts in patients with this condition, in a trial led by Dr Dunbar at the NIH Clinical Center together with other NHLBI investigators. This resulted in the first FDA approval for new drug to treat aplastic anemia in over 30 years. Ongoing clinical trials focus on testing the utility of this drug in other bone marrow failure syndromes.
Biography
Chief, Translational Stem Cell Biology Branch, and Head, Molecular Hematopoiesis Section, National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD.
Dr. Dunbar has pursued a career encompassing clinical investigation and patient care, basic science, and education/administration. As a translational research scientist, she has made important findings in the areas of hematopoiesis, stem cell biology, leukemogenesis, natural killer cell biology, and gene therapies, focusing on non-human primate models to provide insights not possible using murine or in vitro models. She has also led important clinical trials in gene therapy, transplantation, autoimmune disease, and bone marrow failure. She has published over 290 articles in peer-reviewed journals, and served as the principle investigator on numerous clinical protocols. She graduated from Harvard College with a degree in History of Science, and from Harvard Medical School. Following internal medicine training at Boston City Hospital, she came to the NIH as a postdoctoral research fellow in the laboratory of Dr. Arthur Nienhuis, followed by clinical training in hematology at the University of California, San Francisco. In 1991she returned to the NIH to set up her own research program. She has been elected to the American Society for Clinical Investigation, the American College of Physicians and the National Institute of Medicine. She has been active in major professional societies, including current service as the Secretary of the American Society of Hematology, and as past President of the American Society for Cell and Gene Therapy. She served as Editor-in-Chief of the premier hematology journal BLOOD from 2007-2012, the first woman to serve in this position. She has shown great commitment to education and career development of physician-scientists, leading the NIH hematology fellowship program for 17 years. She has been a leader in efforts to enhance the research environment and diversity within the intramural NIH through her service as founding co-chair and current officer of the NIH Assembly of Scientists, and member of the NIH Equity Committee. She has received numerous teaching and mentoring awards from NHLBI, NIH and her professional societies.
Selected Publications
- Kim MY, Yu KR, Kenderian SS, Ruella M, Chen S, Shin TH, Aljanahi AA, Schreeder D, Klichinsky M, Shestova O, Kozlowski MS, Cummins KD, Shan X, Shestov M, Bagg A, Morrissette JJD, Sekhri P, Lazzarotto CR, Calvo KR, Kuhns DB, Donahue RE, Behbehani GK, Tsai SQ, Dunbar CE, Gill S. Genetic Inactivation of CD33 in Hematopoietic Stem Cells to Enable CAR T Cell Immunotherapy for Acute Myeloid Leukemia. Cell. 2018;173(6):1439-1453.e19.
- AlJanahi AA, Lazzarotto CR, Chen S, Shin TH, Cordes S, Fan X, Jabara I, Zhou Y, Young DJ, Lee BC, Yu KR, Li Y, Toms B, Tunc I, Hong SG, Truitt LL, Klermund J, Andrieux G, Kim MY, Cathomen T, Gill S, Tsai SQ, Dunbar CE. Prediction and Validation of Hematopoietic Stem and Progenitor Cell Off-Target Editing in Transplanted Rhesus Macaques. Mol Ther. 2021.
- Olnes MJ, Scheinberg P, Calvo KR, Desmond R, Tang Y, Dumitriu B, Parikh AR, Soto S, Biancotto A, Feng X, Lozier J, Wu CO, Young NS, Dunbar CE. Eltrombopag and improved hematopoiesis in refractory aplastic anemia. N Engl J Med. 2012;367(1):11-9.
- Wu C, Espinoza DA, Koelle SJ, Yang D, Truitt L, Schlums H, Lafont BA, Davidson-Moncada JK, Lu R, Kaur A, Hammer Q, Li B, Panch S, Allan DA, Donahue RE, Childs RW, Romagnani C, Bryceson YT, Dunbar CE. Clonal expansion and compartmentalized maintenance of rhesus macaque NK cell subsets. Sci Immunol. 2018;3(29).
- Dunbar CE, High KA, Joung JK, Kohn DB, Ozawa K, Sadelain M. Gene therapy comes of age. Science. 2018;359(6372).
Related Scientific Focus Areas
This page was last updated on Monday, April 1, 2024